
Misleading: Research on the level and duration of the immune responses from infection and vaccination is still limited. Recovering from a previous infection doesn't guarantee protection against COVID-19.
Inadequate support: There is no sign that face masks harm children; instead, they might reduce the risk of infection and virus spread in schools. No evidence indicates that SARS-CoV-2 was engineered.
Mostly accurate: School closures impact children's educational progress and well-being. Longer intervals between doses strengthen the immune response to mRNA COVID-19 vaccines and reduce side effects.

FULL CLAIM: Natural immunity protects better than vaccination; “the mortality risk of an un-boosted person under age 30 was zero”; cloth face masks, school closures had zero benefits for children and some harm; “Spacing out vaccine doses makes a vaccine more effective and lowers the side effect profile”; Public health officials knew that the virus may have been engineered
REVIEW
On 16 March 2022, Fox News published this opinion article by Marty Makary, a surgical oncologist at Johns Hopkins School of Medicine. In the article, Makary listed what he considered the “10 biggest COVID mistakes” that health authorities made throughout the COVID-19 pandemic regarding public health policies.
According to the social media analytics tool CrowdTangle, the article received more than 15,000 interactions and 2,500 shares on Facebook, and particularly, on Twitter, where Makary shared his article.
This wasn’t the first time that Makary questioned COVID-19 guidance from public health authorities. For example, in a February 2021 opinion piece for the Wall Street Journal, Makary made the claim that the U.S. would reach herd immunity by April 2021, a claim that was unsupported at the time and which turned out to be inaccurate. In a second Wall Street Journal opinion article, he claimed that face masks “increased levels of carbon dioxide in the blood” in children. Health Feedback addressed this claim in earlier reviews (here, here, and here) and found it to be inaccurate as well.
The Fox News article contained several inaccurate, misleading, and unsupported claims, including that face masks harm children, that infection-induced immunity protects better against COVID-19 than vaccination, and that vaccinated adults have zero risk of dying of COVID-19.
Some of the other statements made by Makary are accurate based on our current knowledge about SARS-CoV-2. However, in his criticism of public health policies, Makary also glossed over the complex and rapidly evolving situation in the early stages of the COVID-19 pandemic.
Public health guidelines and decision-making rely on scientific evidence[1]. However, our lack of understanding of a novel virus that threatened to overwhelm healthcare systems compelled public health authorities to often make decisions when faced with a high level of uncertainty. For this reason, evaluating the past policies based on our current and more extensive knowledge of SARS-CoV-2 can be misleading.
Below, we analyze Makary’s science-related claims and provide a summary of the scientific evidence regarding the policies discussed in the article.
Claim 1 (Misleading):
“Natural immunity was 2.8 times better in preventing hospitalization than vaccinated immunity and having both meant you had the same protection as natural immunity alone.”
According to Makary, one of the alleged mistakes was that experts were “ignoring natural immunity”, despite evidence that it provides better protection than vaccination. To support his claim, Makary seemed to refer to a Wall Street Journal opinion piece authored by himself, published on 26 January 2022. This, in turn, cited a study published in Morbidity and Mortality Weekly Report in January 2022[2].
The study evaluated the rate of COVID-19 cases and hospitalizations by vaccination and prior infection status using epidemiological data gathered in New York and California between May and November 2021.
The 2.8 figure that Makary cited corresponded to the period when the Delta variant was predominant. At that time, the study found that the infection and hospitalization rate among unvaccinated, previously infected individuals was around three to four times lower than among vaccinated people with no prior infection.
However, Makary failed to mention that the study showed the opposite trend before the Delta variant emerged. Before the Delta variant, the rate of COVID-19 cases and hospitalizations among unvaccinated, previously infected individuals were two to three times higher than among vaccinated individuals who didn’t have a previous infection.
Therefore, what this study actually showed was that the level of protection conferred by infection or by vaccination varies, as it depends on the period analyzed and the variants circulating in the population at that time. Citing the study as evidence that infection-induced immunity is better than vaccine-induced immunity is a misrepresentation of the study.
Furthermore, the study concluded that vaccination improved protection in previously infected individuals across the entire study period. This contradicts Makary’s claim that vaccination in previously infected individuals didn’t protect more than infection alone. Other studies also observed that vaccination benefits previously infected individuals, providing even stronger immunity against the disease[3,4].
Current evidence on infection-induced and vaccine-induced immunity
Makary didn’t take into account several important factors that might influence a reader’s understanding about infection-induced and vaccine-induced immunity.
First, multiple studies indicate that the immune responses to SARS-CoV-2 infection vary greatly from person to person, depending on factors such as age and disease severity[5-7]. Some people don’t even develop detectable levels of antibodies against the virus. According to data from the U.K. ZOE COVID Study, which analyzes COVID-19 data from a mobile application with more than 4 million users, this could happen in up to one in five previously infected individuals.
Second, the level of protection from infection and vaccination might also depend on the predominant variant at a given time. For example, one preliminary study published in the New England Journal of Medicine analyzed epidemiological data from Qatar and found that previous infection provided less protection against reinfection with the Omicron variant than with other variants[8].
Another study by researchers at Stanford University published in Cell suggested that the antibodies induced by COVID-19 vaccines might better recognize new viral variants than those developed after infection[9].
Finally, the authors of the study in Morbidity and Mortality Weekly Report pointed out that “early declining of vaccine-induced immunity” in individuals who received the vaccine earlier might explain the lower protection observed in vaccinated compared with previously infected individuals during the Delta wave.
Multiple studies show that a booster dose helps strengthen the immune response and enhances vaccine protection against the disease[10-13]. However, the study cited by Makary ended before the widespread rollout of booster doses and couldn’t evaluate their protective effect compared to prior infection.
In short, Makary cherry-picked partial data from a single study as evidence that infection-induced immunity is superior to that obtained through vaccination. While it is clear that both vaccination and prior infection can confer protection against future infection, hospitalization, and death, vaccination is an effective strategy to acquire immunity that is also safer than infection. As Health Feedback explained in this Insight article, both types of immunity aren’t mutually exclusive; vaccination can help previously infected individuals to achieve the best possible protection against the disease.
Claim 2 (Inaccurate):
“A study in the New England Journal of Medicine found that the mortality risk of an un-boosted person under age 30 was zero. You can’t lower a risk of zero any further with a booster.”
Makary cited a study in the New England Journal of Medicine to support his claim that “the mortality risk of an un-boosted person under age 30 was zero”. However, no link to the study was provided; Health Feedback’s attempts to identify the study were unsuccessful.
In November 2021, the U.S. Centers for Disease Control and Transmission (CDC) updated its recommendation for COVID-19 booster doses, stating that all people older than 18 “should” get an extra dose of the COVID-19 vaccine. The decision followed new evidence showing that vaccine effectiveness against infection and severe disease waned over time.
Vaccinated young adults have a lower risk of severe COVID-19 and death than vaccinated people in older age groups and a much lower risk than unvaccinated people of all ages. However, mortality data from the U.S. CDC’s COVID Data Tracker show that 119 vaccinated people aged 18 to 29 (0.6 per 100,000 vaccinated people aged 18 to 29) died in the U.S. from April 2021 through January 2022. Although the mortality rate in vaccinated young people is very low and around half of that for unvaccinated people in the same age group (2,042 deaths or 1.15 per 100,000 unvaccinated people aged 18 to 29), it is clearly not zero. Therefore, Makary’s claim is inaccurate.
Current evidence on the necessity of booster doses in healthy young adults
There was a general consensus in the scientific community that booster doses were necessary for older age groups and other at-risk populations. However, the decision to administer a third dose to healthy young adults was a matter of intense debate, as a New York Times article reported.
Available data showed that young adults remained well protected against severe COVID-19 by primary vaccination[14,15], and many experts believed that an extra dose wouldn’t provide additional benefits. However, the spike in COVID-19 cases driven by the Omicron variant made some experts change their minds and endorse booster doses for young adults as a way to reduce the number of infections and limit the spread of the virus.
According to the U.S. CDC mortality data, 75% of the deaths registered among vaccinated young adults occurred between December 2021 and January 2022, when the Omicron variant became dominant. This likely resulted from the high infection rates caused by Omicron and vaccine immunity waning, suggesting that a booster dose might also benefit this age group.
On 10 March 2022, the U.S. CDC released the first data on the real-world effectiveness of booster doses in the U.S. The data shows that booster doses reduced the likelihood of hospitalization for all age groups, including people aged 18 to 49 (see Figure 1).
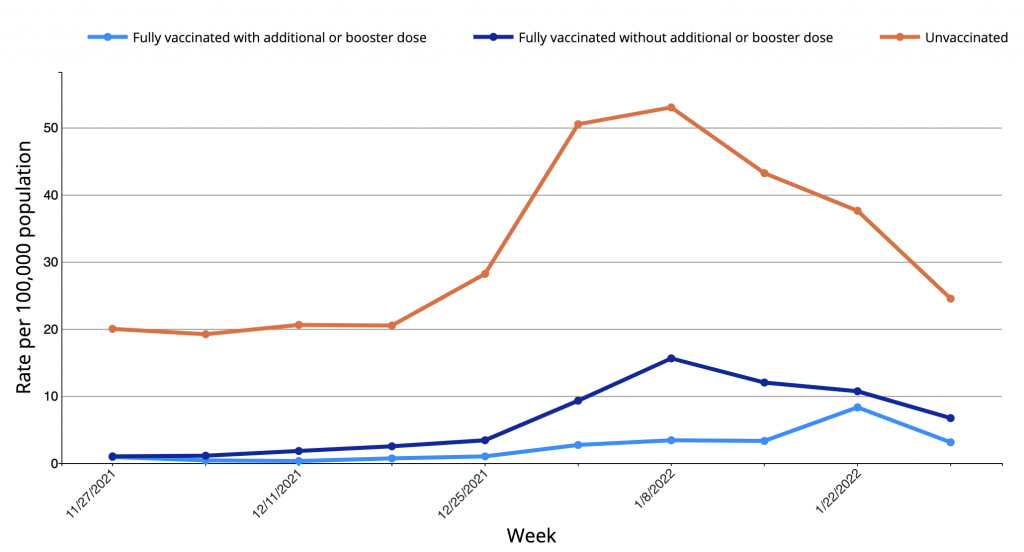
Figure 1. Rates of laboratory-confirmed COVID-19 hospitalizations by vaccination status in adults aged 18 to 49 years between November 2021 and January 2022. Data retrieved on 21 March 2022 from the U.S. CDC’s COVID Data Tracker.
Claim 3 (Lacks context):
“Wash your hands like crazy (at least 20 seconds) and pour alcohol-based solutions on your grocery bags to stop COVID transmission, you were told for months […] The logical starting hypothesis should have been that COVID was aerosolized”
SARS-CoV-2 spreads mainly through respiratory droplets—liquid particles expelled into the air when breathing, talking, or coughing—and through smaller particles called aerosols that can travel further and remain suspended in the air for longer periods of time (airborne transmission).
But transmission through contaminated surfaces or objects (fomites) can also occur. Some studies suggest that a person can get infected by touching surfaces where an ill person recently coughed or sneezed on and then touching the mouth, nose, or eyes[16,17].
The risk of surface transmission is now considered low compared with direct contact and droplet or airborne transmission. However, the exact contribution of surface transmission to infection is difficult to determine because respiratory transmission from an asymptomatic person can’t be ruled out in most cases, as the U.S. CDC website explains.
The mouth, nose, and eyes are very accessible entry routes for harmful microorganisms. Handwashing is a simple preventive measure and is associated with a lower risk of SARS-CoV-2 infection[18]. Even if surface transmission accounts for only a small proportion of the infections, handwashing reduces this risk by adding an extra layer of protection.
Evidence about airborne transmission at earlier and later stages of the pandemic
In the early days of the pandemic, public health authorities assumed that SARS-CoV-2 spread mainly through respiratory droplets and contaminated surfaces, not through aerosols. While handwashing and surface disinfecting were understandable precautionary measures, many scientists criticized the long time it took public health authorities to acknowledge the airborne transmission of SARS-CoV-2.
In mid-2020, there were already reports of several outbreaks compatible with transmission through aerosols. This evidence led 239 scientists to co-sign an open letter in July 2020 urging public health agencies to review their guidance. As a result of the newly emerged evidence, both the U.S. CDC and the World Health Organization acknowledged the possibility of airborne transmission under certain circumstances.
Claim 4 (Inadequate support):
“Current data suggests that covering the faces of children for two years with a cloth mask had zero benefit and some harm”
The claim that wearing a face mask is detrimental for children is unsupported by current evidence. The American Academy of Pediatrics (AAP) explains that face masks are safe and effective for anyone over two years old and that wearing a face mask doesn’t interfere with breathing, lung development, and the immune system. Such claims have no scientific basis and have been debunked multiple times by Health Feedback (here, here, and here) and others (here, here, and here).
There is also no evidence supporting the claim that face masks negatively affect children’s development, as Health Feedback explained in this earlier review. Experts in child development explained in an article in National Geographic that, while face masks do hide some cues involved in learning and social interaction, they are unlikely to cause long-term negative effects because children can easily adapt to use alternative cues.
In contrast, available evidence suggests that face masks provide benefits for children. The most evident one is reducing the risk of infection. Children have a very low risk of becoming seriously ill with COVID-19. However, some still develop severe COVID-19 or die, as shown in a March 2022 joint report from the AAP and the Children’s Hospital Association. In addition, some suffer complications like Multisystem Inflammatory Syndrome or experience persistent symptoms[19].
Furthermore, by reducing SARS-CoV-2 transmission, face masks might provide another indirect but very important benefit to children by helping to keep schools open. For example, one study that surveyed childcare professionals from all 50 U.S. states found that a consistent use of face masks by children two years and older in childcare settings reduced the risk of childcare program closure by 14%[20].
Current evidence on the effectiveness of face masks in reducing school infections
As explained above, SARS-CoV-2 spreads mainly through respiratory droplets and aerosols. When the more contagious Omicron variant emerged, many countries recommended the use of N95 respirators, particularly in high-risk settings. Respirators filter aerosols much more effectively than cloth or surgical masks, preventing the release of infectious material by infected people and protecting the wearer. But as Health Feedback explained in an earlier review, cloth masks still reduce the risk of infection in certain settings by preventing infected people from releasing respiratory droplets[21]. This is known as source control.
This science brief from the U.S. CDC summarizes multiple scientific studies that support community mask-wearing for reducing the spread of SARS-CoV-2, particularly when combined with additional protective measures, such as vaccination and adequate ventilation. Research on the effectiveness of mask-wearing specifically in school settings is scarce and produced mixed results. But evidence summaries from the U.S. CDC and the U.K. Department for Education concluded that mask-wearing by staff and students helped limit the spread of the virus in schools, as Health Feedback explained in an earlier review.
Claim 5 (Mostly accurate):
“Now studies are revealing the catastrophic harm [of school closure] to a generation of children – significant motor and cognitive declines and a mental health crisis.”
The uncertainty about the impact of COVID-19 in children and their role in SARS-CoV-2 transmission led many countries, including the U.S., to close schools in early 2020 to limit viral spread. The duration of these closures in the U.S. varied substantially among states, but the measure was a subject of intense debate since attending school is critical to children’s academic and social development.
Our current knowledge of the virus indicates that the epidemiological benefits of school closures are unlikely to outweigh their harmful consequences for the students. A February 2022 article in The Conversation highlighted the impact of pandemic-related school closures, such as reduced educational progress, increased risk of school dropout, and poorer physical and emotional well-being. Therefore, the AAP now favors layered prevention and control strategies, leaving school closures only as a last resort.
Current evidence on the effectiveness of school closures to reduce the spread of SARS-CoV-2
Determining the specific contribution of schools to SARS-CoV-2 transmission is challenging because it is influenced by other factors like the rate of infection in the general population and the use of control measures in schools. Even two years after the start of the pandemic, it remains unclear how much schools contribute to the spread of the virus, and studies show mixed results.
For example, one study conducted in the U.S. between March and May 2020 found that school closures were temporarily associated with decreased COVID-19 incidence and mortality[22]. The effect was more pronounced in states that closed schools earlier, when the number of COVID-19 cases was still low.
In contrast, another study comparing closed upper-secondary schools and open lower-secondary schools in Sweden found that transmission within open schools was very limited for students and their parents[23]. However, the impact on teachers was much higher, and the number of infections among them almost doubled.
In March 2022, the Norwegian Institute of Public Health published a more recent study in the journal Pediatrics. The study compared students’ infection rates over time in open and closed schools from seven boroughs in Oslo[24]. The results showed that school closure wasn’t more effective than targeted prevention and control measures in reducing infection rates.
Overall, the scientific evidence illustrates how Makary’s opposition to school closures and the measures that could prevent school closures are incompatible with each other.
Claim 6 (Accurate):
“Spacing out vaccine doses makes a vaccine more effective and lowers the side effect profile. It also would have allowed the U.S. to save more lives when we were rationing a scarce vaccine supply.”
On 22 February 2022, the U.S. CDC updated its recommended COVID-19 vaccination schedule by increasing the interval between mRNA vaccine doses from three to eight weeks. The update was in response to new research showing that delaying the second dose of the mRNA vaccines increased antibody responses and might lower the risk of myocarditis in adolescents and young adults. The change didn’t apply to high-risk populations like immunocompromised people and people over 65, who were still recommended to follow a three-week interval.
Makary‘s article said that “public health officials dismissed pleas to space out the doses as many of us called for”. In fact, delaying the second dose of COVID-19 vaccine had been a matter of discussion since the rollout of the COVID-19 vaccine, given the short supply of COVID-19 vaccines at that time. When Makary called for longer intervals between doses in September 2021, preliminary data already suggested that spacing the doses might increase the antibody response[25], as a June 2021 article in The Conversation acknowledged.
However, evidence supporting longer intervals between doses wasn’t always so clear. When the U.K. chose to increase the interval between vaccine doses up to a maximum of 12 weeks in January 2021, the decision was criticized by the British Medical Association, reported The Guardian. The same report also cited the World Health Organization (WHO), which warned there was no scientific evidence for delays longer than six weeks, and some experts feared that delaying the second dose would reduce vaccine effectiveness. Furthermore, delaying the second dose left people partially unprotected for a longer time, at a moment when the number of cases was rising.
Claim 7 (Unsupported):
“The singular focus on vaccines meant that little attention was paid to lifesaving therapeutics”
Fighting COVID-19 requires both vaccines that reduce the risk of infection and disease and treatments that improve the survival and recovery of those who get ill. Therefore, developing safe and effective COVID-19 vaccines and treatments were a priority since the start of the pandemic. But vaccines provide additional benefits because they reduce a person’s risk of disease and its associated risks, and they also reduce the spread of the virus in the community, as Health Feedback explained in this review.
Developing effective COVID-19 treatments proved more elusive than getting a vaccine, particularly in the case of early treatments. However, the claim that the vaccine was the cause isn’t supported by evidence. This July 2021 article in Science News pointed instead to other factors, including the efforts dedicated to drugs that ultimately turned out to be false leads like hydroxychloroquine, the difficulty of recruiting non-hospitalized COVID-19 patients for clinical trials, and the narrow spectrum of patients that could benefit from a single therapy.
Furthermore, the U.S. Food and Drug Administration (FDA) created the Coronavirus Treatment Acceleration Program (CTAP) in April 2020, contradicting the claim that research on therapies was set aside. This special program aimed at moving new treatments to patients “as quickly as possible, while at the same time finding out whether they are helpful or harmful”.
Makary’s article specifically mentioned two treatments, Pfizer’s oral antiviral Paxlovid, also called nirmatrelvir, and the antidepressant medication fluvoxamine. The first one demonstrated an 88% reduction in COVID-19 hospitalization and death in clinical trials when used within five days of symptom onset[26]. On 22 December 2021, the U.S. FDA authorized the emergency use of Paxlovid for the treatment of mild-to-moderate COVID-19 patients older than 12 who are at high risk of severe COVID-19.
In contrast, current treatment guidelines don’t recommend using fluvoxamine in COVID-19 patients. While a few studies showed that fluvoxamine might reduce the risk of hospitalization[27-29] and the World Health Organization is considering it as a candidate for COVID-19 therapeutics, the evidence for its use is still limited and inconclusive.
Research on COVID-19 treatments
Currently, several COVID-19 treatments are available in the U.S. and other countries. These include anti-inflammatory drugs that reduce excessive immune response to the virus, antivirals that prevent viral replication inside the cells, and antibody therapies that mimic our immune response and attack the virus (monoclonal antibodies).
In the early stages of the pandemic, researchers had to address the critical need for life-saving treatments in cases of severe COVID-19. This led to the discovery that the anti-inflammatory corticosteroid dexamethasone reduced COVID-19 deaths in patients with severe COVID-19 and it remains the most effective treatment available so far. However, better therapies that benefit a broader range of patients are still needed.
At the time of this review’s publication, hundreds of ongoing COVID-19 trials are testing new drugs, as well as drugs that are already approved for other medical conditions. This article in Nature summarizes the most promising candidates as of 22 March 2022.
Claim 8 (Inaccurate):
“Prominent U.S. virologists told Drs. Fauci and Francis Collins of their concern that the virus may have been manipulated and originated in the lab, but then suddenly changed their tune in public comments days after meeting with the NIH officials. The virologists were later awarded nearly $9 million from Fauci’s agency”
In June 2021, Washington Post and Buzzfeed News filed a Freedom of Information Act (FOIA) request on Fauci’s official correspondence from the first half of 2020. Among the thousands of emails released in response to the request, there was one that Kristian G. Andersen, a professor of immunology and microbiology at Scripps Research Institute, wrote to Anthony Fauci, the director of the U.S. National Institute of Allergy and Infectious Diseases, on 31 January 2020.
In his email, Andersen said that the genetic analysis suggested that bats served as SARS-CoV-2 reservoir and “one has to look really closely at all the sequences to see that some of the features (potentially) look engineered”. He added, “But we have to look at this much more closely and there are still further analyses to be done, so those opinions could still change”.
Makary’s claim may be a reference to that exchange, which some interpreted as evidence that SARS-CoV-2 was engineered (see example here). However, Health Feedback reviewed the claim and found it to be inaccurate, because Andersen only expressed uncertainty about the possible engineering of the virus, not definite evidence favoring this hypothesis. In fact, Andersen and colleagues continued studying the genetic sequence of the virus. They published their results in Nature Medicine on 17 March 2020[30], concluding that “Our analyses clearly show that SARS-CoV-2 is not a laboratory construct or a purposefully manipulated virus.”
Andersen explained his change of mind regarding the origin of the virus in a Twitter thread on 4 June 2021. He said that new evidence, including the release of the genomes of related coronaviruses, indicated that SARS-CoV-2 arose naturally:
“All the features in SARS-CoV-2 that, to us, suggested possible engineering were identified in related coronaviruses in the first half of 2020, which largely invalidated our preliminary hypothesis of engineering and instead bolstered the argument for a natural origin.”
Therefore, the claim that SARS-CoV-2 was known to be possibly engineered based on Andersen’s email is unsupported and a misrepresentation of the email exchange.
Current evidence on the origin of the virus
The evidence so far indicates that the virus’s genome is consistent with a natural origin and doesn’t show signs of engineering[31]. Therefore, the general consensus held by experts is that the virus most likely arose naturally.
Three preprints—a preprint is a manuscript that hasn’t been peer-reviewed by other scientists yet—published in early 2022, offer additional evidence that SARS-CoV-2 may have jumped from animals to humans in the Wuhan market. If true, analyzing samples taken from the species sold in the market might allow scientists to identify the animal species that carried the virus in the first place.
Although there is no evidence showing that SARS-CoV-2 leaked from a lab, there is also no evidence to rule it out at the moment. This possibility isn’t mutually exclusive with a natural origin for the virus. In the meantime, scientists continue investigating the origin of SARS-CoV-2.
Conclusion
Makary’s article contains a mix of accurate, inaccurate, unsupported, and misleading claims about the COVID-19 pandemic. Taken together, they convey the message that public health response to COVID-19 wasn’t informed by evidence. This is misleading and fails to account for the complexity of public health decision-making when scientific data is scarce or unavailable.
The many uncertainties during the early stages of the pandemic meant that public health policies kept changing as new evidence arose. Some of those policies may be viewed now as mistakes, and scientific research will tell us whether some were. Evaluating the effectiveness public health response to COVID-19 can help us improve our preparedness for future pandemic threats.
REFERENCES
- 1 – Brownson et al. (2009) Understanding Evidence-Based Public Health Policy. American Journal of Public Health.
- 2 – Leon et al. (2022) COVID-19 Cases and Hospitalizations by COVID-19 Vaccination Status and Previous COVID-19 Diagnosis — California and New York, May–November 2021. Morbidity and Mortality Weekly Report.
- 3 – Wang et al. (2021) Naturally enhanced neutralizing breadth against SARS-CoV-2 one year after infection. Nature.
- 4 – Stamatatos et al. (2021) mRNA vaccination boosts cross-variant neutralizing antibodies elicited by SARS-CoV-2 infection. Science.
- 5 – Tomic et al- (2022) Divergent trajectories of antiviral memory after SARS-CoV-2 infection. Nature Communications.
- 6 – Chia et al. (2021) Dynamics of SARS-CoV-2 neutralising antibody responses and duration of immunity: a longitudinal study. The Lancet Microbe.
- 7 – He et al. (2021) Seroprevalence and humoral immune durability of anti-SARS-CoV-2 antibodies in Wuhan, China: a longitudinal, population-level, cross-sectional study. The Lancet.
- 8 – Altarawneh et al. (2022) Protection against the Omicron Variant from Previous SARS-CoV-2 Infection. The New England Journal of Medicine.
- 9 – Röltgen et al. (2022) Immune imprinting, breadth of variant recognition, and germinal center response in human SARS-CoV-2 infection and vaccination. Cell.
- 10 – Ferdinand et al. (2022) Waning 2-Dose and 3-Dose Effectiveness of mRNA Vaccines Against COVID-19–Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance — VISION Network, 10 States, August 2021–January 2022. Morbidity and Mortality Weekly Report.
- 11 – Tartof et al. (2022) Effectiveness of a third dose of BNT162b2 mRNA COVID-19 vaccine in a large US health system: A retrospective cohort study. The Lancet Regional Health Americas.
- 12 – Thompson et al. (2022) Effectiveness of a Third Dose of mRNA Vaccines Against COVID-19–Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance — VISION Network, 10 States, August 2021–January 2022. Morbidity and Mortality Weekly Report.
- 13 – Andrews et al. (2022) Effectiveness of COVID-19 booster vaccines against COVID-19-related symptoms, hospitalization and death in England. Nature Medicine.
- 14 – Tartof et al. (2021) Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: a retrospective cohort study. The Lancet.
- 15 – Self et al. (2021) Comparative Effectiveness of Moderna, Pfizer-BioNTech, and Janssen (Johnson & Johnson) Vaccines in Preventing COVID-19 Hospitalizations Among Adults Without Immunocompromising Conditions — United States, March–August 2021. Morbidity and Mortality Weekly Report.
- 16 – Bae et al. (2020) Asymptomatic Transmission of SARS-CoV-2 on Evacuation Flight. Emerging Infectious Diseases.
- 17 – Xi et al. (2020) The evidence of indirect transmission of SARS-CoV-2 reported in Guangzhou, China. BMC Public Health.
- 18 – Doung-ngern et al. (2020) Case-Control Study of Use of Personal Protective Measures and Risk for SARS-CoV 2 Infection, Thailand. Emerging Infectious Diseases.
- 19 – Molteni et al. (2021) Illness duration and symptom profile in symptomatic UK school-aged children tested for SARS-CoV-2. The Lancet Child and Adolescent Health.
- 20 – Murray et al. (2022) Association of Child Masking With COVID-19–Related Closures in US Childcare Programs. JAMA.
- 21 – Andrejko et al. (2022) Effectiveness of Face Mask or Respirator Use in Indoor Public Settings for Prevention of SARS-CoV-2 Infection — California, February–December 2021. Morbidity and Mortality Weekly Report.
- 22 – Auger et al. (2020) Association Between Statewide School Closure and COVID-19 Incidence and Mortality in the US. JAMA.
- 23 – Vlachos et al. (2021) The effects of school closures on SARS-CoV-2 among parents and teachers. PNAS.
- 24 – Rotevatn et al. (2022) School Closure Versus Targeted Control Measures for SARS-CoV-2 Infection. Pediatrics.
- 25 – Parry et al. Extended interval BNT162b2 vaccination enhances peak antibody generation. NPJ Vaccines.
- 26 – Hammond et al. (2022) Oral Nirmatrelvir for High-Risk, Nonhospitalized Adults with Covid-19. New England Journal of Medicine.
- 27 – Reis et al. (2022) Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial. The Lancet Global Health.
- 28 – Seftel et al. (2021) Prospective Cohort of Fluvoxamine for Early Treatment of Coronavirus Disease 19. Open Forum Infectious Diseases.
- 29 – Lenz et al. (2020) Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients With Symptomatic COVID-19. A Randomized Clinical Trial. JAMA.
- 30 – Andersen et al. (2020) The proximal origin of SARS-CoV-2. Nature Medicine.
- 31 – Holmes et al. (2021) The origins of SARS-CoV-2: A critical review. Cell.


