
FULL CLAIM: “There's a ‘spike’ in [COVID-19] cases because there's a spike in testing.”
REVIEW
Dozens of Facebook posts circulated on social media in late June and early July 2020 claiming that the spike in the number of reported COVID-19 cases in the U.S. during the second half of June 2020 was due to increased testing, and not to an increased number of infections. However, increases in both the proportion of tests returning a positive result and the number of hospital visits during this period indicate that the claim is inaccurate.
The U.S. saw a surge in identified cases of COVID-19 in June 2020. While this could be a sign that the epidemic is regaining steam following the reopening of some states, some people have claimed that the surge is a mere artifact of increased testing. They suggest that a more comprehensive virological survey of the population via increased testing would naturally detect more infected people, including asymptomatic ones. This, they claim, would in turn give a false impression that COVID-19 is spreading more quickly.
Indeed, increased testing will identify more cases. However, in order to determine whether the rate of spread of COVID-19 is increasing, we must look at the proportion of positive test results (also known as the positivity rate) rather than raw numbers of cases. In June 2020, this proportion of tests returning a positive result began to increase again (see below).
If the epidemic were declining, an increase in the number of tests conducted should result in a decrease in the positivity rate. This is because the number of infected people in the population would be declining at the same time that more uninfected individuals would be receiving testing. For example, if the number of new infections in a population of 1,000 decreases from 500 to 250 per day, and at the same time, testing capacity is increased from 1,000 per day to 1,200, the positivity rate would go from 50% to about 20%.
In the case of a stable epidemiological situation, in which the circulation of the virus among the population is not changing, an increase in the number of tests among the general population would not change the proportion of individuals who test positive. In other words, the positivity rate would remain constant. To give a hypothetical example, if a given population of 1,000 has 100 infected (10% of the population), a testing of a random sample of 100 people in that population would return 10 positive tests (10 persons infected). This would yield a positivity rate of 10%. If, say, 300 more people from the population were then randomly selected to be tested, this sampling would statistically include 30 more infected. The result of the new testing campaign with higher testing capacity (300 tests) would then also yield a 10% positivity rate (30 positive tests for 300 total).
These examples demonstrate that an increase in testing does not necessarily influence the positivity rate. They also demonstrate that the U.S. would not be seeing an increase in the positivity rate of COVID-19 testing unless the epidemic was spreading.
To analyze the behavior of the positivity rate over time, Health Feedback aggregated the total number of COVID-19 tests and the number of positive results reported by public health laboratories, clinical laboratories, and commercial laboratories and collected by the U.S. Centers for Disease Control and Prevention (CDC). The data indicate that the positivity rate began to increase in June (Figure 1). This means that the proportion of infected people detected by the tests is increasing during this period, indicating that the virus is spreading.
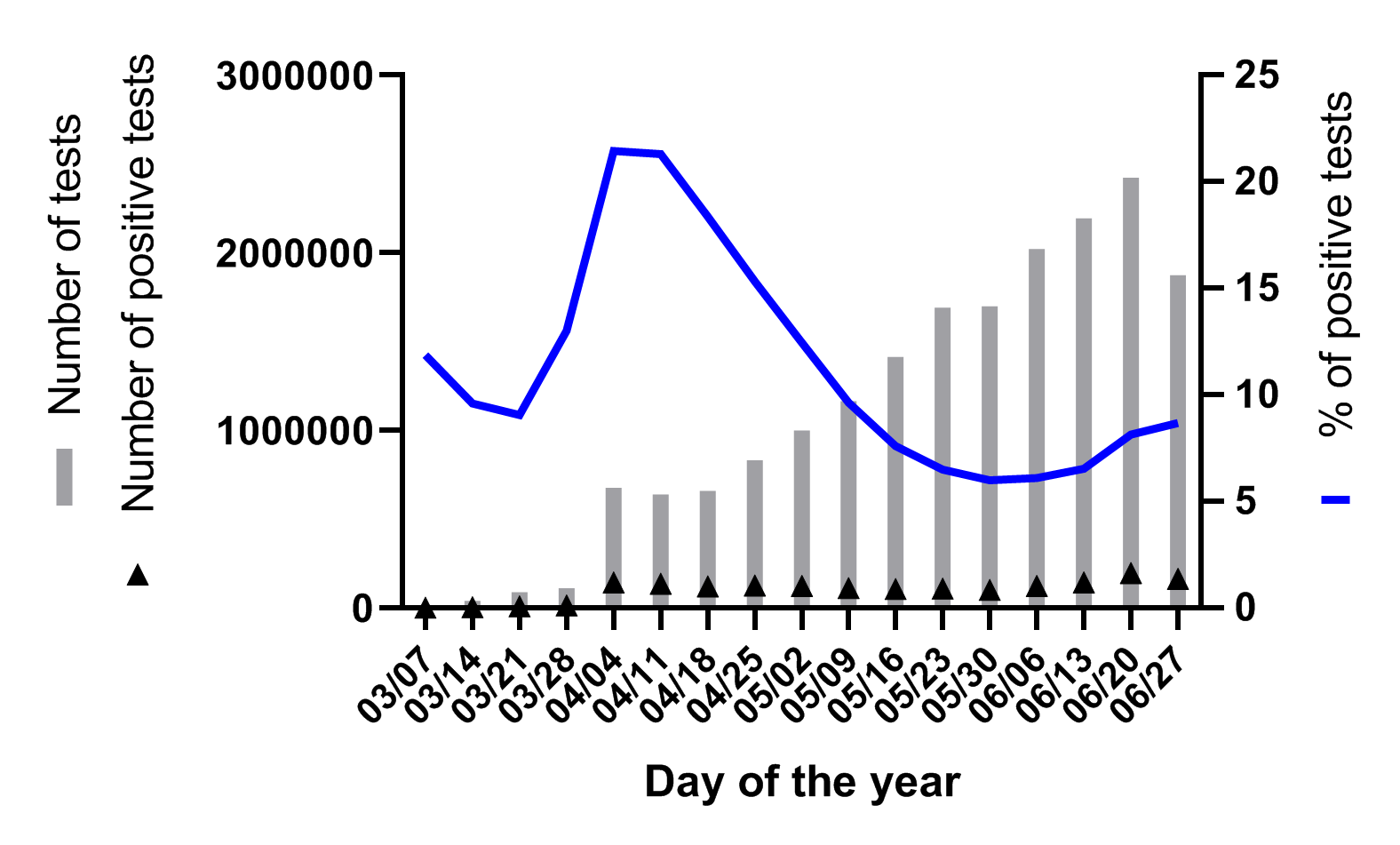
In addition, we can observe that the total number of tests performed has increased steadily since the week ending 18 April. If the increased number of positive tests was a direct consequence of performing more tests, we would expect to see a rise in the proportion of positive tests starting 18 April, but this is not the case.
One possible reason that the positivity rate did not increase with increased testing is that the population being tested was not a random sample from the total population (sampling bias). For example, if the tests were only performed on people who show clear signs and symptoms of COVID-19, then the positivity rate would skyrocket, even if disease transmission among the general population had not significantly changed. If this was the case, then increasing the overall number of tests could lead to a biased positivity rate that does not reflect disease prevalence in the community.
To address the potential issue of a biased positivity rate, we can look at the number of hospital visits due to symptoms resembling those of COVID-19 (fever and cough or shortness of breath or difficulty breathing) as provided by the CDC. As shown in Figure 2, after having declined from late March to early June, the number of hospital visits related to COVID-19-like symptoms once again increased. In other words, the second half of June has seen a surge in people reaching out to hospitals for treatment of respiratory illness. This therefore indicates that the observed increase in COVID-19 cases is not a mere statistical artifact and reflects an actual increase in the proportion of people who are sick from COVID-19.
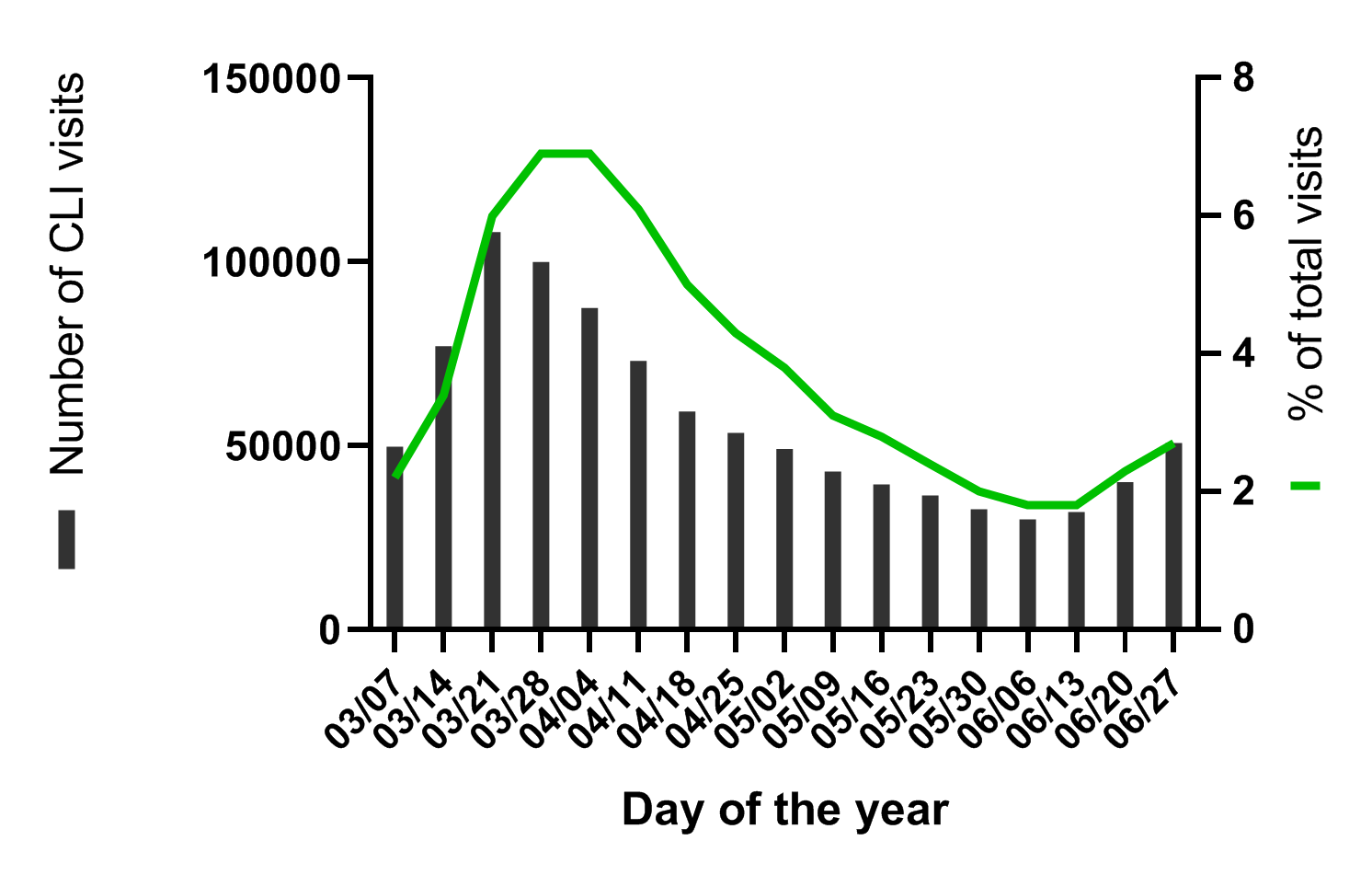
In summary, the proportion of COVID-19 positive cases has risen during the second half of June 2020. This shows that the spike in COVID-19 observed in the U.S. in June 2020 was not simply due to an increase in the number of tests performed. If the spread of COVID-19 in the U.S. were in fact stable or declining, the proportion of tests returning a positive result would have either remained constant or decreased, but they did not. Furthermore, data from hospitals indicate that more people have sought medical attention due to respiratory illness. The claim that the surge in COVID-19 cases is a mere artifact of increased testing which gives the false impression that the rate of COVID-19 infection is increasing is therefore inaccurate.
READ MORE
The claim that the surge in COVID-19 cases was due to increased testing was also investigated by PolitiFact, which found it to be inaccurate.
An epidemiologist from the University of Arizona told FactCheck.org that “community transmission is increasing, and that increasing case counts are not simply an artifact of testing”.