
Lack of context: The level of protection from infection varies depending on multiple factors, such as a person’s age and the severity of the disease. Vaccination tends to generate a more consistent response, at least in certain populations like the elderly. In addition, it can enhance the immunity acquired through infection.

FULL CLAIM: “natural immunity provides superior protection to experimental vaccines; “They lied and said Natural Immunity wasn’t better than [vaccine]-induced immunity”
REVIEW
As COVID-19 vaccines became widely available, most countries implemented vaccine requirements to help limit the spread of SARS-CoV-2. This measure triggered an intense social debate about why previously infected people would still need to get vaccinated. But infection-induced immunity—often referred to as “natural immunity”—was also championed by those opposing vaccine mandates, who often presented this type of immunity as “superior” and incompatible with that induced by vaccination.
This narrative was revived in mid-February 2023 (examples here, here, and here) by the publication of a study in The Lancet, authored by researchers from the Institute for Health Metrics and Evaluation and the Department of Global Health at the University of Washington. The study concluded that infection-induced immunity “appears to be at least as durable, if not more so, than that provided by two-dose vaccination with the mRNA vaccines”[1].
Prominent individuals such as U.S. Senator Rand Paul, interpreted the results of the Lancet study as evidence that the public had been lied to about the protection conferred by a previous infection, which some attributed to an intent of monetizing the pandemic. Similarly, an article by the anti-vaccine organization Children’s Health Defense claimed that “vaccines are failing” and “The Lancet is finally acknowledging […] that natural immunity provides superior protection to experimental vaccines”.
Other users, like Member of U.K. Parliament Andrew Bridgen, went further and accused public health authorities of intentionally exposing people to the alleged “high” risks of COVID-19 vaccines despite knowing they provided no benefit.
Posts on Facebook, Instagram, and Twitter mentioning the Lancet study and the term “natural immunity” in such a manner received more than 250,000 interactions, according to social media analytics tool CrowdTangle. The study alone received over 25,000 interactions and 3,000 shares on these platforms.
Contrary to what the article in Children’s Health Defense claimed, COVID-19 vaccines demonstrated their safety and efficacy in clinical trials before use in the public and therefore aren’t experimental. Apart from that, claims that infection provides “better” protection against COVID-19 than vaccination are misleading in several ways that we detail below.
What did the Lancet study show?
The Lancet study analyzed data from 65 previous studies in 19 countries to estimate how infection with different SARS-CoV-2 variants reduced the risk of reinfection, symptomatic disease, and severe disease (hospitalization and death) compared to people who had never been infected.
The results showed that previously infected individuals were, on average, 85% less likely to develop severe disease from any variant than individuals who were never infected, and this protection lasted for almost a year. However, infection with the Omicron BA.1 variant was less protective against reinfection (45%) and also immunity waned more rapidly (36% at 49 weeks post-infection) compared to the original strain or the Alpha, Beta, and Delta variants (82% protection, declining to 78.6% at 40 weeks post-infection).
For every variant, the level and duration of the protection induced by a previous infection seemed comparable to that acquired after two doses of an mRNA vaccine (Figure 1).
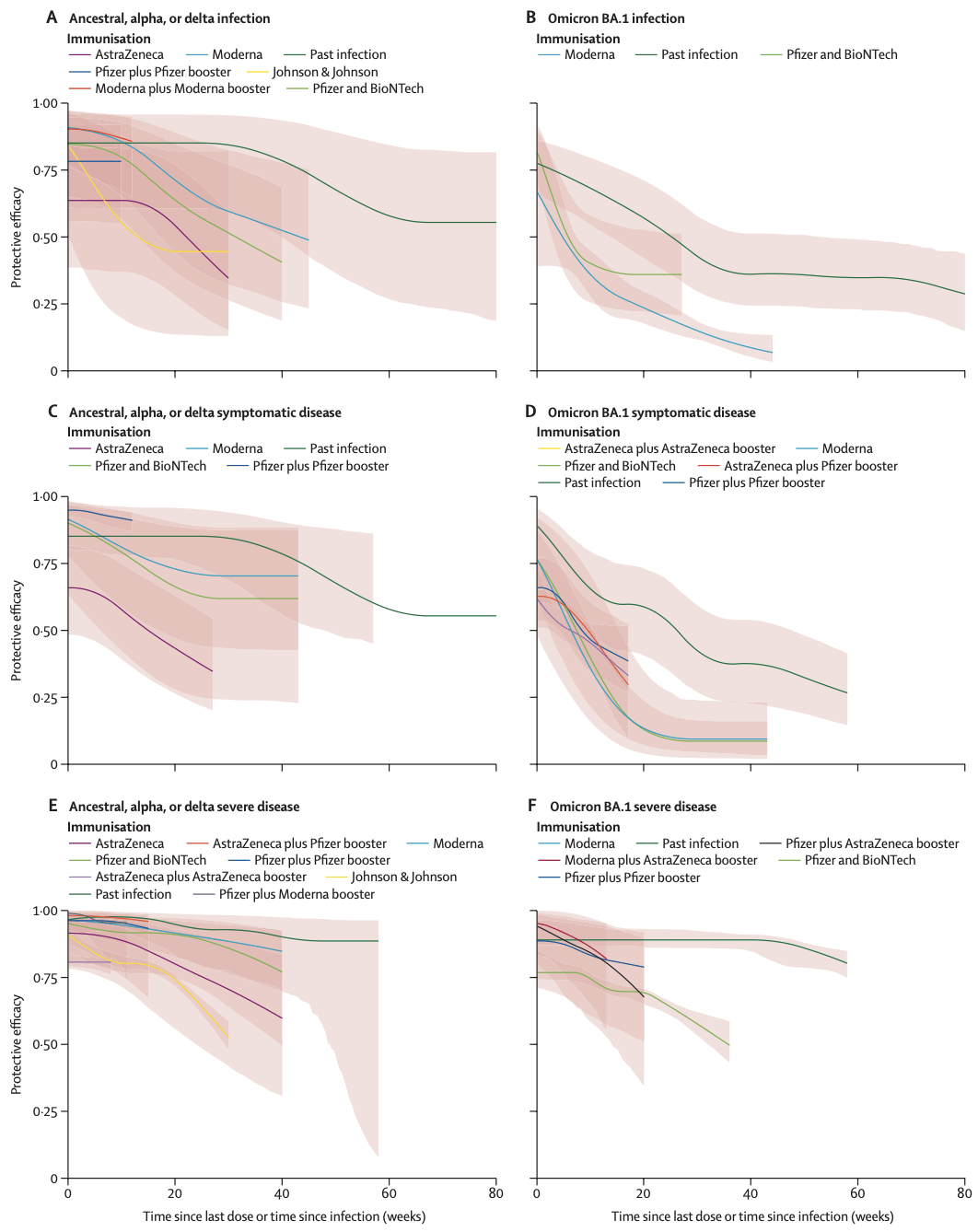
Figure 1. Protection efficacy from past COVID-19 infection compared to protection from vaccination (by vaccine type and dose) against re-infection, symptomatic disease, and severe disease for ancestral, alpha, delta, and Omicron BA.1 variants. The pink shading represents the uncertainty intervals, which are a measure of the variability among different individuals. The wider this shading is, the less confidence we can have in the estimate[1].
While the results of the study suggest that the level of protection from a past infection is similar to that induced by two doses of an mRNA COVID-19 vaccine, the authors pointed out that this protection must be evaluated in the context of the risks:
“Protection from past infection in comparison with that conferred by vaccination, however, must be weighed against the risks of severe morbidity and mortality associated with the initial infection. This balance of risk varies by the type of variant, with omicron for instance having less severe outcomes than delta, and other risk factors associated with the individual, such as age and other comorbidities.”
Infection-induced immunity comes at a price
There is no question that both infection and vaccination protect against future reinfection and disease to some degree. But regardless of how strong and durable infection-induced immunity is, getting infected exposes the person to the risks of the disease. This is precisely what we wish to avoid in the first place, because the price of this exposure is one that we can’t predict in advance.
Although most COVID-19 cases are mild, some people develop complications, including lung and heart problems, blood clots, and kidney damage[2-4]. Some of these people don’t survive the disease, as evidenced by the more than 6.8 million deaths that COVID-19 has caused worldwide. Around one-third of those who survive continue to experience symptoms months after recovering from the initial infection[5], a condition called long COVID. These persistent symptoms include fatigue, difficulty breathing, and difficulty thinking clearly, which can greatly impact the person’s quality of life.
Furthermore, new evidence indicates that the risk of adverse health conditions in multiple organs might increase with repeated SARS-CoV-2 infections[6], highlighting the importance of preventing exposure to the virus and not relying on infection-induced immunity for protection.
Posts like this tweet by Bridgen suggested that the known risks of the vaccines outweigh their benefits. However, such a claim is misleading because it presents the risks of vaccination as unacceptable even though we know SARS-CoV-2 infection poses a much greater risk of serious complications, especially for the elderly and people with underlying health conditions. For example, while mRNA COVID-19 vaccines—the main COVID-19 vaccines used in the U.S. and Europe—are indeed associated with a slightly higher risk of heart inflammation, this risk is higher after SARS-CoV-2 infection[7]. Overall, the risk of serious side effects following COVID-19 vaccines is extremely small when compared to the disease.
In short, while a person can develop immunity through both infection and vaccination, COVID-19 vaccines are a much safer strategy for acquiring immunity because they are very safe and don’t expose the person to the potential risks of the disease, as the authors of the study highlighted on a Twitter thread:
Another thing to consider is that evaluating past policies based on current and more extensive evidence can be misleading because scientific evidence informing policies evolves as researchers gather new data and knowledge. While the Lancet study strongly suggests now that infection and vaccination might provide a similar level of protection against a new encounter with the virus, most of this evidence wasn’t available some months before.
Contradicting claims made by some social media users that infection-induced immunity wasn’t recognized by the authorities, multiple countries, including the U.S. and many European countries, did accept proof of recovery from a recent SARS-CoV-2 infection as an alternative to proof of vaccination.
Furthermore, the claim that scientists and public health authorities denied “the reality” of infection-induced immunity is inaccurate. Since early in the pandemic, public health authorities acknowledged that people who recovered from a past infection developed some degree of immunity, but data about the strength and durability of this protection was limited.
Maria Van Kerkhove, epidemiologist and technical lead for the COVID-19 response at the WHO, explained in December 2020:
“When individuals are infected with the SARS-CoV-2 virus, the virus that causes COVID-19, they develop antibodies a few weeks after infection. We know that individuals who have even severe disease, mild disease, and even asymptomatic infection, do develop these antibodies. Studies are underway to show us how strong this immune response is and for how long these antibodies last […] some see some studies showing that they last for six months and possibly longer. But we do have clues from other coronaviruses, that it will not be a lifelong immunity.”
Previous infection doesn’t guarantee protection against COVID-19
The results from the Lancet study showed that infection provides protection comparable to that of vaccination. However, whether the immune protection following infection is actually higher or more durable than after vaccination as some users claimed is unclear, as we need to consider some nuances.
For example, while the study showed that the estimated protection tends to be higher after infection than after vaccination in the mid-term, vaccination seems to provide higher protection against severe disease from Omicron than infection during the first 20 weeks (see above graph F in Figure 1).
It’s also important to keep in mind that scientists are able to study infection-induced immunity for a much longer period than vaccine-induced immunity, simply because COVID-19 vaccines only arrived on the scene a year after the pandemic started. Hence previously infected individuals were generally followed up for longer periods (up to 60 to 80 weeks) than vaccinated individuals (up to 20 to 40 weeks).
In other words, contrary to what some social media users claimed, the longer lines of past infection don’t mean that protection from infection lasts longer, but that we have more of a headstart on studying infection-induced immunity than vaccine-induced immunity. To figure out whether vaccination provides protection on a comparable timescale as infection, we need more time.
In addition, the results of the study tell us that the immune protection from either infection or vaccination can vary greatly depending on the variant. Notably, protection is lower against the Omicron variant compared to previous variants. But one important limitation of the study is that it didn’t analyze the latest Omicron subvariants currently dominant in the U.S. and worldwide because data on these subvariants were scarce or unavailable at the time of the study. Therefore, the study doesn’t show how well a previous infection will protect us against these variants.
Although not included in the analysis, the study cited a few individual studies showing that infection with the BA.2, BA.4, and BA.5 subvariants conferred a lower level of protection compared to earlier variants, including Omicron BA.1[8-11]. The protection against these subvariants was further reduced when the previous infection was from a pre-Omicron variant than when it was from an earlier Omicron subvariant. Considering these data and the fact that the newest Omicron subvariants are increasingly transmissible and more capable of evading immunity than BA.1, we can’t simply assume that infection with one variant will protect us against any future variant.
The Lancet study also acknowledged several limitations, including a relatively small number of studies available for the analysis, differences in the way each study defined past infection and COVID-19 hospitalization, and scarce data on protection against severe disease.
Finally, as an article by the Children’s Hospital of Philadelphia explained, people who recovered from COVID-19 can develop variable degrees of immunity, depending on factors such an age and disease severity. In this context, choosing to rely exclusively on infection-induced immunity can be risky as some previously infected people will remain nonetheless susceptible to the disease[12].
Certainly, Omicron subvariants are also better at evading immunity from vaccination than previous variants, and vaccine protection can also vary from person to person depending on factors like age[13]. However, unlike infection, vaccination involves a controlled exposure, and current evidence indicates that it tends to generate a more consistent immune response than previous infection, at least in certain populations like older adults and people with underlying health conditions[14,15].
One study published in the American Journal of Public Health in January 2023 underscored the real-world benefits of vaccination. The study, which analyzed more than 260,000 vaccine recipients and the same number of previously infected individuals in the U.S. state of Indiana, found that the rate of SARS-CoV-2 infection at six months was higher in the vaccinated compared to those previously infected[16].
However, vaccinated people had lower rates of all-cause emergency visits, hospitalizations, and mortality compared to previously infected individuals, particularly older adults. The authors attributed the higher risk in previously infected people to the health consequences of the exposure to SARS-CoV-2.
In summary, getting infected not only exposes the person to the risks of the disease, but also doesn’t guarantee that the person is well protected against future infection and disease. While vaccination is also not 100% effective, it adds an extra layer of protection for those who recovered from COVID-19 and might or might not have developed immunity.
Vaccination enhances protection in previously infected individuals
Arguing which type of immunity is “better” as some social media users did creates a false dichotomy by incorrectly presenting infection and vaccination as mutually exclusive options when they aren’t, as Health Feedback discussed in an earlier Insight article.
Multiple studies showed that receiving a dose of a COVID-19 vaccine enhances the immune protection in previously infected individuals[17,18]. This combined immunity resulting from infection and vaccination is known as “hybrid immunity”. While the Lancet study didn’t analyze the effect of vaccination in previously infected individuals, earlier studies showed that hybrid immunity provides a more robust and durable protection against infection, hospitalization, and severe disease from the Omicron variant than infection or vaccination alone[19,20].
These data underscore the benefits of vaccination even in previously infected individuals and support the recommendation by public health authorities like the U.S. Centers for Disease Control and Prevention that individuals who recovered from COVID-19 should also get vaccinated.
Conclusion
Both infection and vaccination can protect against COVID-19. However, claims that infection-induced immunity is “superior” to that provided by COVID-19 vaccines fail to acknowledge that vaccination is a much safer way of acquiring immunity because it doesn’t require exposing the person to the risks of the disease. While infection can induce robust and durable immunity, often more than vaccination, the level of protection it confers varies from person to person depending on factors such as age and disease severity. Therefore, recovering from COVID-19 doesn’t guarantee that the person will be protected against the disease.
Overall, the debate over which type of immunity is “better” ultimately oversimplifies the complexity of the immune system. The fact is that a person’s level of immunity depends on the SARS-CoV-2 variants that are dominant at that time and on the individual’s own state of health. It also assumes incorrectly that immunity from infection and vaccination are mutually exclusive, rather than complementary. The current evidence indicates that vaccination enhances immunity from a previous infection and is the best way to minimize future risks in people who have recovered from the disease.
READ MORE
Oncologist David Gorski analyzed in an article for Science-Based Medicine the narrative vindicating “natural immunity”, which the article describes as a “deceptive simplification of a complex issue”.
This infographic by the British Society for Immunology and the U.K. Coronavirus Immunology Consortium explains the similarities and differences in immunity against COVID-19 gained through SARS-CoV-2 infection compared to vaccination.
REFERENCES
- 1 – Stein et al. (COVID-19 Forecasting Team) (2023) Past SARS-CoV-2 infection protection against re-infection: a systematic review and meta-analysis. The Lancet.
- 2 – Farshidfar et al. (2021) Cardiovascular complications of COVID-19. Journal of Clinical Investigation Insight.
- 3 – Knight et al. (2022) Association of COVID-19 With Major Arterial and Venous Thrombotic Diseases: A Population-Wide Cohort Study of 48 Million Adults in England and Wales. Circulation.
- 4 – Nadim et al. (2020) COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup. Nature Reviews Nephrology.
- 5 – Chen et al. (2022) Global Prevalence of Post-Coronavirus Disease 2019 (COVID-19) Condition or Long COVID: A Meta-Analysis and Systematic Review. Journal of Infectious Diseases.
- 6 – Bowe et al. (2022) Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nature Medicine.
- 7 – Pantone et al. (2022) Risk of Myocarditis After Sequential Doses of COVID-19 Vaccine and SARS-CoV-2 Infection by Age and Sex. Circulation.
- 8 – Altarawneh et al. (2022) Protective Effect of Previous SARS-CoV-2 Infection against Omicron BA.4 and BA.5 Subvariants. New England Journal of Medicine.
- 9 – Chemaitelly et al. (2022) Protection of Omicron sub-lineage infection against reinfection with another Omicron sub-lineage. Nature Communications.
- 10 – Andeweg et al. (2022) Protection of COVID-19 vaccination and previous infection against Omicron BA.1, BA.2 and Delta SARS-CoV-2 infections. Nature Communications.
- 11 – Carazo et al. (2022) Protection against omicron (B.1.1.529) BA.2 reinfection conferred by primary omicron BA.1 or pre-omicron SARS-CoV-2 infection among health-care workers with and without mRNA vaccination: a test-negative case-control study. The Lancet Infectious Diseases.
- 12 – Gudbjartsson et al. (2020) Humoral Immune Response to SARS-CoV-2 in Iceland. New England Journal of Medicine.
- 13 – Bates et al. (2022) BNT162b2-induced neutralizing and non-neutralizing antibody functions against SARS-CoV-2 diminish with age. Cell Reports.
- 14 – Karachaliou et al. (2022) SARS-CoV-2 infection, vaccination, and antibody response trajectories in adults: a cohort study in Catalonia. BMC Medicine.
- 15 – Binu et al. (2023) Comparison of infection-induced and vaccine-induced immunity against COVID-19 in patients with cirrhosis. Hepatology.
- 16 – Tu et al. (2023) SARS-CoV-2 Infection, Hospitalization, and Death in Vaccinated and Infected Individuals by Age Groups in Indiana, 2021‒2022. American Journal of Public Health.
- 17 – Wang et al. (2021) Naturally enhanced neutralizing breadth against SARS-CoV-2 one year after infection. Nature.
- 18 – Stamatatos et al. (2021) mRNA vaccination boosts cross-variant neutralizing antibodies elicited by SARS-CoV-2 infection. Science.
- 19 – Bobrovitz et al. (2023) Protective effectiveness of previous SARS-CoV-2 infection and hybrid immunity against the omicron variant and severe disease: a systematic review and meta-regression. The Lancet Infectious Diseases.
- 20 – Malato et al. (2023) Stability of hybrid versus vaccine immunity against BA.5 infection over 8 months. The Lancet Infectious Diseases.


