
Misleading: While both infection and vaccination can generate some protective immunity, vaccination is safer because it does so without exposing the person to the risks associated with the disease. While lauding the benefits of infection-induced immunity, the article glossed over the fact that those who die from COVID-19 don’t develop immunity at all.
FULL CLAIM: “Natural Immunity Better Than Protection From COVID-19 Vaccination”; “People who recovered from COVID-19 were better off than those who received a COVID-19 vaccine, researchers find”
REVIEW
Like with most pathogens that enter the body, infection with SARS-CoV-2 confers some protection against future encounters with the virus. This infection-induced immunity—often called “natural immunity”—has been repeatedly invoked as an argument against COVID-19 vaccination and vaccine mandates.
Any new piece of evidence showing that a past infection protects against COVID-19 has been wielded as evidence that immunity from infection is “better” than that from vaccination. This claim resurfaced in late November 2023 with a study conducted in Estonia and published in Scientific Reports[1].
Headlines proclaiming the superiority of infection-induced immunity based on this study appeared in the Washington Times and The Epoch Times. The Epoch Times’ article was reproduced on other websites, including ZeroHedge and The Blaze, which also posted about the study on social media. This tweet by ZeroHedge received over one million views.
However, these headlines are misleading because they convey the message that getting infected is a better strategy for acquiring immunity than vaccination or that those who recover from infection don’t need to get vaccinated. Neither of these messages are true, as this review will show.
Hybrid immunity, not infection, offered the best protection
The study by Uusküla et al. is a retrospective cohort study. This type of study uses existing health data over a period of time to examine the relationship between a given exposure and the health outcome of interest.
Specifically, Uusküla et al. evaluated the level of protection from previous infection and COVID-19 vaccination (exposures) using data from the Estonian national health system from 23 February 2020 to 25 June 2022. As a measure of protection, the researchers analyzed the risk of infection and hospitalization (outcomes).
The researchers then compared these risks in people who had recovered from infection with people with no immunity (Cohort 1, n = 94,982), hybrid immunity resulting from previous infection and vaccination (Cohort 2, n = 47,342), and people who had received a COVID-19 vaccine (Cohort 3, n = 254,920).
The results showed that people who recovered from an infection were around five times less likely to have a new infection and ten times less likely to become hospitalized compared to those who had never been infected. This protection lasted for over a year during the period when the Delta variant was dominant. The researchers also found that people who recovered from a SARS-CoV-2 infection had a lower risk of reinfection (Figure 1) and hospitalization compared to vaccinated people.
These results suggest that infection-induced immunity generally offers “stronger and longer-lasting protection against infection, symptoms, and hospitalization compared to vaccine-induced immunity”.
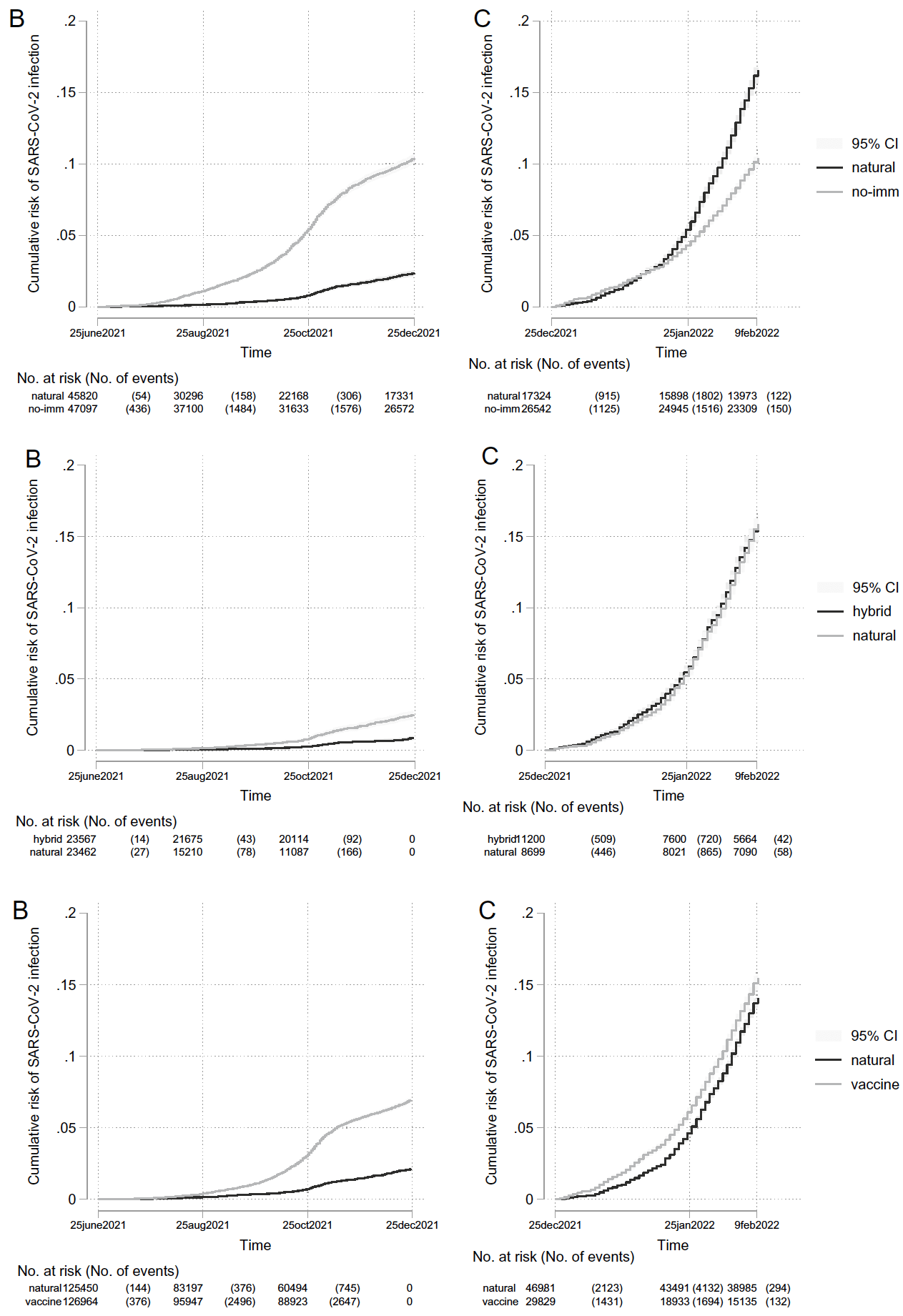
Figure 1 – Comparison of the cumulative risk of SARS-CoV-2 infection (Y-axis) through time (X-axis) in people with infection-induced immunity versus no immunity (Cohort 1, top), hybrid immunity (Cohort 2, middle), and vaccine-induced immunity (Cohort 3, bottom). In each row, the graph on the left (B) shows the period when the Delta variant was dominant, while the graph on the right (C) shows the period when the Omicron variant was dominant.
However, what the headlines didn’t mention is that hybrid immunity conferred the best protection against both infection (Figure 1) and hospitalization. In fact, the researchers found that protection from hybrid immunity against severe illness “significantly exceeded that of natural immunity”. The authors noted that “hospitalization was extremely rare among individuals with hybrid immunity”.
Thus, the key takeaway from this study would be that hybrid immunity offers the best protection against infection and serious illness. This highlights the fact that infection and vaccination aren’t mutually exclusive options, as the debate about which-type-of-immunity-is-better suggests. The study’s results clearly show that people who recovered from a past infection can also benefit from vaccination.
Finally, the authors also acknowledged several limitations of the study. These included potential misclassification—of individuals who had a SARS-CoV-2 infection but weren’t tested—and confounding factors. Although the study corrected for potential confounders such as sex, education, and underlying health conditions, the different groups studied might differ in other characteristics that the authors didn’t control for, including health-seeking behavior, that might have influenced the results.
Not every individual who recovers from an infection develops protection
Many factors can influence how well a person fights an infection and the level of immunity this person develops. Differences in age, genetics, underlying health conditions, and severity of the first infection can lead to variable levels of protection.
In addition, research has shown that the SARS-CoV-2 variant that caused the infection also determines the level of protection against other variants. For example, a past infection provides relatively good protection against reinfection with Alpha, Beta, and Delta variants. However, the Omicron variant is better able to evade immunity from previous infection and vaccination compared to other variants so far[2-4].
In line with these observations, the study by Uusküla et al. showed that while a past infection conferred good protection against reinfection with the Delta variant, this protection vanished during the period when the Omicron variant was dominant. In fact, those who had an infection were surprisingly 25% more likely to become infected during the Omicron wave compared to those who had never been infected. In contrast, vaccinated people had half that risk (13%) during the same period.
The authors speculated that this effect might be explained by the characteristics of the Omicron variant—more transmissible and less virulent than previous variants—and by differences in the characteristics of the population exposed to this variant, including age and exposure behavior.
In summary, one cannot simply assume that a past infection provides consistent and reliable protection against future infection. Given the many factors that can influence immunity, some individuals might develop reasonably good protection, whereas others will remain susceptible to reinfection and illness. Likewise, while infection-induced immunity might offer better protection in some circumstances, vaccination might prove more protective in others.
In this context, vaccination added an extra layer of protection for people who’d recovered from infection. This helps ensure the person has the best possible protection rather than relying solely on infection-induced immunity. That is why public health authorities like the U.S. Centers for Disease Control and Prevention (CDC) recommend that previously infected individuals also receive a COVID-19 vaccine.
It is also fair to acknowledge that, in the early stages of the pandemic, evidence about the protection provided by infection-induced immunity was lacking or very scarce. In contrast, large clinical trials demonstrated the safety and efficacy of COVID-19 vaccines. Therefore, vaccine requirements were based on the best scientific evidence available at the time.
Infection is a much riskier pathway to immunity than vaccination
One aspect often overlooked when comparing the protective effect of infection and vaccination is the potential risks that infection inevitably carries.
For example, the study by Uusküla et al. didn’t mention the severity of the first infection in the group of infection-induced immunity nor how many of them developed long-term COVID-19 complications, such as organ damage and long COVID.
But more importantly, the study only included individuals who recovered from infection, leaving out those who didn’t survive (survivorship bias). During the study period, Estonia confirmed almost 2,500 COVID-19 deaths. While this number might seem small, in a country with a population of only 1.3 million, it means that roughly one in 500 people died before developing immunity.
Therefore, those willing to gain immunity through infection face various risks that also need to be considered in the risk-benefit analysis of infection-induced immunity. Health Feedback discussed this issue in a previous Insight article.
While vaccination also carries some risks, these are minimal compared to the risks of infection. Large clinical studies have shown that COVID-19 vaccines are generally safe[5-8]. Cases of serious adverse events, including blood clotting and heart inflammation, are very rare and don’t outweigh the benefits of vaccination.
In other words, while both infection and vaccination provide immunity, vaccination does so in a much safer way because it doesn’t expose the person to the risks of the disease.
Conclusion
There is no question that recovering from a SARS-CoV-2 infection can provide some protection against disease. The study by Uusküla et al. showed that this protection can even exceed that of COVID-19 vaccines. However, vaccination remains the safest strategy for acquiring immunity because it offers protection without exposing the person to the risks of infection, including serious illness, long-term complications, and death.
It’s also important to account for nuances regarding infection-induced immunity and that getting infected doesn’t guarantee the same protection for everyone. How much a past infection protects against future infection depends on the individual and the variant that caused the infection. This means some people who recovered from an infection could still remain insufficiently protected against the disease. But vaccination enhances this protection, reducing even further the risk of reinfection and serious illness.
REFERENCES
- 1 – Uusküla et al. (2023) Risk of SARS-CoV-2 infection and hospitalization in individuals with natural, vaccine-induced and hybrid immunity: a retrospective population-based cohort study from Estonia. Scientific Reports.
- 2 – Liu et al. (2022) Striking antibody evasion manifested by the Omicron variant of SARS-CoV-2. Nature.
- 3 – Cao et al. (2021) Omicron escapes the majority of existing SARS-CoV-2 neutralizing antibodies. Nature.
- 4 – COVID-19 Forecasting Team (2023) Past SARS-CoV-2 infection protection against re-infection: a systematic review and meta-analysis. The Lancet.
- 5 – Munro et al. (2021) Safety and immunogenicity of seven COVID-19 vaccines as a third dose (booster) following two doses of ChAdOx1 nCov-19 or BNT162b2 in the UK (COV-BOOST): a blinded, multicentre, randomised, controlled, phase 2 trial. The Lancet.
- 6 – Klein et al. (2021) Surveillance for Adverse Events After COVID-19 mRNA Vaccination. JAMA.
- 7 – Barda et al. (2021) Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting. New England Journal of Medicine.
- 8 – Polack et al. (2020) Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. New England Journal of Medicine.


