
Lack of context: HBV infection is often asymptomatic. Despite intensive screening for HBV in pregnant women, some cases might still be missed. This makes universal vaccination at birth essential to prevent transmission from mothers to infants, who have the highest risk of developing long-term complications or dying from hepatitis B.
FULL CLAIM: “hepatitis B is a blood-borne disease that you get if you are an intravenous drug user or if you are sexually promiscuous […] the only other reason that a baby, a newborn baby, would get hepatitis B is if the mom has it”; “If you don't have hepatitis B then your baby's not going to have hepatitis B”; “there's 16 times the amount of aluminum that the FDA says can poison a baby”
REVIEW
Childhood routine immunizations are essential to protect children’s health. Vaccination helped eliminate many potentially disabling and life-threatening infectious diseases that were common in the U.S. in the pre-vaccine era, including polio, smallpox, and measles. Thus, vaccines have greatly contributed to increasing life expectancy at birth and improving the population’s overall health, as Health Feedback explained earlier in this review.
Despite these evident benefits, some parents still avoid vaccinating their children due to misconceptions about infectious diseases and vaccine safety. One example is a YouTube video posted by political commentator Liz Wheeler, where she cited several reasons for declining to vaccinate her newborn daughter against hepatitis B. This vaccine is part of the childhood immunization schedule recommended by the U.S. Centers for Disease Control and Prevention (CDC).
The video received more than 9,900 views on YouTube, and over 12,500 interactions on Facebook and Twitter, according to the social media analytics tool CrowdTangle.
In the video, Wheeler claimed that hepatitis B vaccination in newborns is unsafe and unnecessary unless the mother has an Hepatitis B Virus (HBV) infection. She further claimed that the vaccine fails to achieve its only benefit, which would be to prevent infection “by the time [vaccinated individuals] might become sexually active”. As we will explain below, these claims are incorrect.
Furthermore, the video misrepresents both the scientific reasons and the primary goal of hepatitis B vaccination in newborns, which is to prevent infection during early childhood, when the risk of long-term health problems and death from the disease is highest.
Below, we will address Wheeler’s claims and explain what hepatitis B is, how it is transmitted, and what is the scientific evidence behind universal infant vaccination against this disease.
Hepatitis B is an incurable and potentially life-threatening disease
Hepatitis B is a form of liver inflammation caused by HBV. Most people who get a new HBV infection, called acute infection, have mild or no symptoms. However, some people experience more severe symptoms, including yellowing of the skin or eyes, extreme fatigue, nausea, and vomiting that may require hospitalization. In some cases, acute hepatitis can lead to acute liver failure, a condition that can be fatal or require liver transplantation.
While most people clear the virus on their own within six months, some develop a chronic infection. According to the U.S. Department of Health and Human Services, an estimated 862,000 people had chronic hepatitis B in the U.S. in 2016. This condition poses a serious health risk that can lead to long-term health problems, including cirrhosis, liver cancer, and even death.
There is no treatment for acute hepatitis B. For people who develop chronic infection, oral antivirals are available to slow the progression and prevent liver damage, but they can’t cure the disease, and most people who start treatment must continue it for life. Therefore, prevention remains the only available strategy against the disease.
People who don’t belong to at-risk groups can also get infected; young children have the highest risk of developing chronic hepatitis B and die
Anyone who has an acute or chronic hepatitis B infection can transmit the virus to others through their blood, semen, or other body fluids such as saliva, tears, or urine[1,2]. Transmission occurs when an infectious fluid gets in contact with open cuts or sores or the mucosae of a non-infected person. But contact isn’t limited to only direct interaction with infected individuals, because the virus can survive and remain infectious outside the body for at least seven days, according to the U.S. CDC website.
In the U.S., groups considered at risk for HBV infection include workers at risk for exposure to blood, people who inject drugs, HIV-positive persons, household contacts of persons with HBV infection, men who have sex with men, and people from countries with high levels of HBV infection, among others. Most of the infections in the U.S. occur through injected drug use, sexual contact, and transmission from an infected mother to her baby during pregnancy or at birth.
Wheeler claimed that there is no reason to vaccinate newborns when the mother didn’t test positive for HBV because “hepatitis B is a blood-borne disease that you get if you are an intravenous drug user or if you are sexually promiscuous, neither of which my newborn daughter was”. However, this claim is incorrect. First, some estimates suggest that prevention programs that screen for HBV infections in pregnant women, like the U.S.-funded Perinatal Hepatitis B Prevention Program, don’t capture all the expected babies born to women with HBV infection[3]. Second, other transmission routes are also possible, even during childhood.
Transmission during surgical procedures, dialysis, transfusion, and household or child-to-child transmission are uncommon in regions with low HBV circulation but can still occur. In fact, child-to-child transmission is a major route of infection in regions with high HBV transmission because children are more likely to have contact with each other’s body fluids, such as saliva and tears.
The age at which the person gets infected with HBV is one of the main factors that determine the disease’s outcome. Only 2 to 6% of the people who became infected as adults develop chronic hepatitis B, according to the website of the U.S. CDC. In contrast, the infection becomes chronic in around 90% of infants and 30% of children below six[4]. Up to 25% of infants infected at birth will die prematurely of HBV-related causes. That is why prevention during early childhood is crucial.
Furthermore, children are less likely to show symptoms than adults, increasing the risk of remaining undiagnosed and untreated. The asymptomatic nature of many HBV infections also facilitates virus transmission because people might be unaware of the infection and don’t take measures to prevent transmission to others.
One study from the Polaris Observatory—an initiative that provides resources supporting the elimination of Hepatitis B—published in The Lancet Gastroenterology and Hepatology estimated that only 10% of global HBV infections that occurred during 2016 were diagnosed, and only 5% of the individuals eligible for treatment actually received it[5]. A similar trend applies to the U.S., as Figure 1 shows.
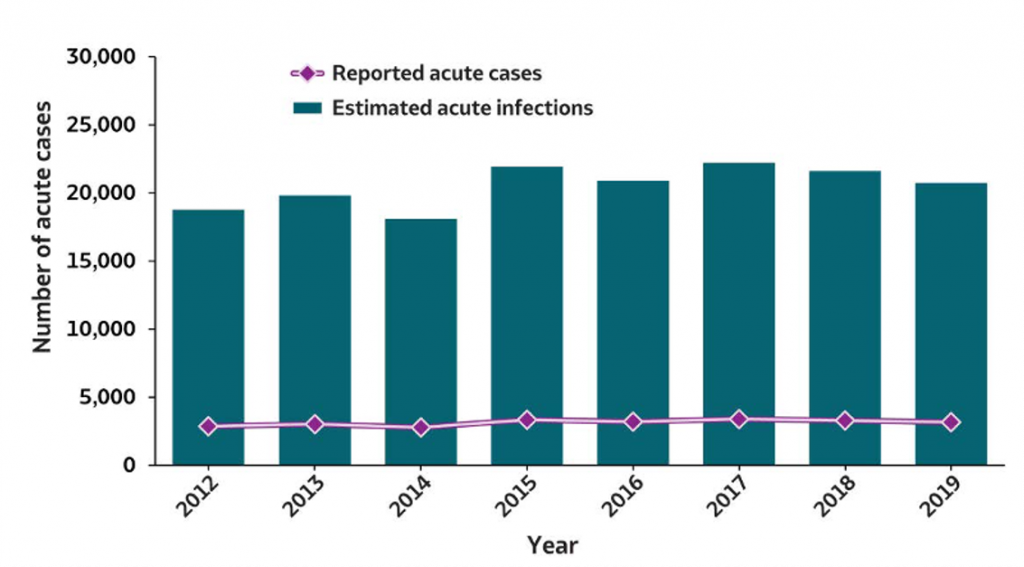
Figure 1. Number of reported acute hepatitis B virus infections and estimated infections in the U.S. between 2012 and 2019. Source: U.S. CDC’s viral hepatitis surveillance 2019 report.
Therefore, while certain groups are at a much higher risk of getting an HBV infection, the risk for the rest of the population, including young children, isn’t zero, as Wheeler suggested. In fact, data from the U.S. CDC shows that around 30% of the hepatitis B infections reported in the U.S. in 2019 weren’t associated with any high-risk behavior or exposure (see Figure 2).
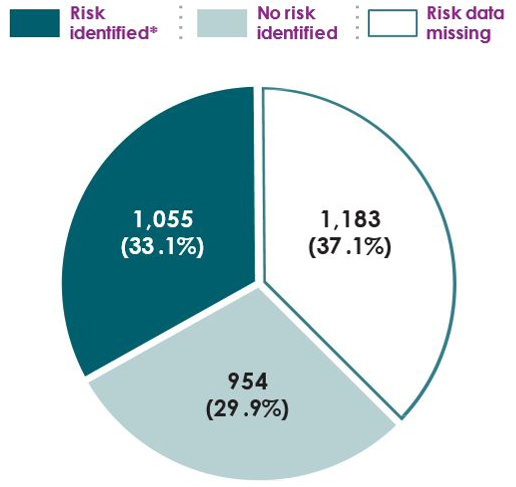
Figure 2. Reported cases of acute HBV infection in the U.S. in 2019 based on exposure to at least one identified risk within the six months before developing symptoms or getting a positive HBV test result. Risk data missing refers to cases in which investigations were not possible due to the loss of follow-up or lack of resources to conduct the investigations. Figure modified from U.S. CDC’s viral hepatitis surveillance 2019 report.
Hepatitis B vaccines are safe and highly effective; universal childhood vaccination has proven more effective than strategies targeting at-risk populations
Wheeler’s idea that hepatitis B vaccination should focus exclusively on those groups at risk of infection had already been tested and proven ineffective during the first hepatitis B vaccine rollout in the U.S. in 1982. During almost a decade, this targeted approach failed to lower the incidence of the disease. The main reason was that identifying individuals engaged in high-risk behaviors or exposures before they became infected was generally unfeasible. Furthermore, many people who didn’t belong to high-risk groups and were therefore not targeted for vaccination still got infected[6].
In 1991, the U.S. ACIP changed its strategy and recommended universal childhood vaccination, extending it to all people under 19 in 1999. As a result, the rate of reported acute HBV infections in the U.S. declined by 67% between 1990 and 2002. Among the population under 19, the decrease was 89%. These data contradict Wheeler’s claim and show that universal vaccination at birth is a very effective strategy to reduce HBV infections[7].
The World Health Organization and the U.S. CDC currently recommend universal hepatitis B vaccination in a three-dose scheme, starting within 24 hours after birth. This prevents the potential risk that mothers with undocumented HBV infections transmit the virus to their babies. A single dose of the hepatitis vaccine administered within 24 hours after birth is 70 to 95% effective at preventing perinatal HBV infection from an infected mother to her baby[8,9].The complete vaccination series is 80 to 100% effective at preventing HBV infection and clinical hepatitis B[10].
The U.S. CDC website summarizes multiple safety studies showing that the hepatitis B vaccines are also safe, contrary to what Wheeler claimed in the video.
Specifically, Wheeler claimed that the hepatitis B vaccines contain “16 times the amount of aluminum that the FDA says can poison a baby”. One possible origin for this claim is a 2018 article by James Lyons-Weiler and Robert Ricketson, claiming that “On Day 1 of life, infants receive 17 times more aluminum than would be allowed if doses were adjusted per body weight”, suggesting that this amount exceeds safe aluminum levels. However, they didn’t provide any experimental or other scientific evidence to support their claim, as these two articles on Respectful Insolence and Skeptical Raptor explained. Lyons-Weiler previously spread vaccine misinformation and Ricketson has a history of medical malpractice.
Claims that vaccines are unsafe based on the alleged toxicity of their ingredients, including aluminum, are incorrect. As Health Feedback explained in earlier reviews, some vaccines contain aluminum salts as an adjuvant, which is an enhancer of the immune response to vaccination.
Aluminum salts are very common in nature, and small amounts of aluminum are present in the air, food, and drinking water. While aluminum salts in excessive amounts may cause some side effects such as nausea, vomiting, or diarrhea, the tiny amounts present in vaccines are safe. The hepatitis B vaccines approved for use at birth contain less than 0.5 mg of aluminum per dose. As the Children’s Hospital of Philadelphia explains on its website, these amounts are minimal compared to the amount that infants receive in their regular diet[11].
Finally, Wheeler claimed that hepatitis B vaccines missed their goal because “only 24% of teenagers who had been immunized with hepatitis B at birth were still immunized by the time they were in high school”. This claim is inaccurate and misleading. As explained above, one of the primary goals of vaccination is to prevent infection during the most vulnerable ages of early childhood.
Furthermore, epidemiological and immunological data indicate that hepatitis B vaccines likely provide long-term protection[12,13]. One study published in the Journal of Infectious Diseases showed that around 50% of the vaccinated individuals had protective antibody levels 30 years after the primary vaccination series, and up to 94% might retain some degree of immunity[12]. Furthermore, hepatitis B vaccination was also associated with a reduced risk of all-cause and cancer-related mortality 20 years later[13]. For this reason, public health authorities like the WHO don’t recommend booster vaccinations for persons who have completed the three-dose vaccination schedule.
Conclusion
Hepatitis B is an incurable life-threatening disease. Contrary to Wheeler’s claims, no one has a zero risk of getting infected, even during childhood. Prevention is the only available strategy against hepatitis B, and it is particularly important during early childhood, when the risk of developing long-term complications and even dying from the disease is highest. Universal hepatitis B vaccination at birth provides safe and effective long-term protection against infection and chronic disease. This strategy has proven much more effective in reducing HBV infections in the overall population than targeted vaccination of at-risk groups.
UPDATE (04 April 2022):
This review was updated to cite a 2018 article by Lyons-Weiler and Ricketson as the possible origin of Wheeler’s claim that hepatitis B vaccines contain “16 times the amount of aluminum that the FDA says can poison a baby”.
REFERENCES
- 1 – Komatsu et al. (2012) Tears From Children With Chronic Hepatitis B Virus (HBV) Infection Are Infectious Vehicles of HBV Transmission: Experimental Transmission of HBV by Tears, Using Mice With Chimeric Human Livers. Journal of Infectious Diseases.
- 2 – Heiberg et al. (2010) Hepatitis B Virus DNA in Saliva from Children with Chronic Hepatitis B Infection. Implications for Saliva as a Potential Mode of Horizontal Transmission. The Pediatric Infectious Disease Journal.
- 3 – Koneru et al. (2019) Estimating Annual Births to Hepatitis B Surface Antigen–Positive Women in the United States by Using Data on Maternal Country of Birth. Public Health Reports.
- 4 – Paganelli et al. (2012) Chronic hepatitis B in children and adolescents. Journal of Hepatology.
- 5 – The Polaris Observatory Collaborators. (2018) Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. The Lancet Gastroenterology and Hepatology.
- 6 – Alter et al. (1990) The Changing Epidemiology of Hepatitis B in the United States
Need for Alternative Vaccination Strategies. JAMA. - 7 – Villiers et al. (2021) The impact of the timely birth dose vaccine on the global elimination of hepatitis B. Nature Communications.
- 8 – Stevens et al. (1985) Perinatal Hepatitis B Virus Transmission in the United States
Prevention by Passive-Active Immunization. JAMA. - 9 – Poovorawan et al. (1989) Protective Efficacy of a Recombinant DNA Hepatitis B Vaccine in Neonates of HBe Antigen—Positive Mothers. JAMA.
- 10 – Szmuness et al. (1980) Hepatitis B Vaccine — Demonstration of Efficacy in a Controlled Clinical Trial in a High-Risk Population in the United States. New England Journal of Medicine.
- 11 – Mitkus et al. (2011) Updated aluminum pharmacokinetics following infant exposures through diet and vaccination. Vaccine.
- 12 – Bruce et al. (2016) Antibody Levels and Protection After Hepatitis B Vaccine: Results of a 30-Year Follow-up Study and Response to a Booster Dose. The Journal of Infectious Diseases.
- 13 – He et al. (2021) The impact of hepatitis B vaccination in the United States, 1999–2018. Hepatology.


