
Overstates scientific confidence: Although scientists have discovered that previous infections with common coronaviruses can produce memory T cells which recognize the virus SARS-CoV-2, we still do not know whether the presence of these cells are associated with protection from COVID-19. It is therefore premature to claim that these cells confer pre-existing immunity.

FULL CLAIM: “The overall lethality of [COVID-19] (IFR) is about 0.1% to 0.3% and thus in the range of a severe influenza”; “up to 60% of all persons may already have a certain cellular background immunity to the new coronavirus due to contact with previous coronaviruses (i.e. cold viruses)”; “There is still little to no scientific evidence for the effectiveness of cloth face masks in healthy and asymptomatic individuals”...
REVIEW
An article on a website named Swiss Policy Research, formerly Swiss Propaganda Research, claims to give readers the “Facts about [COVID-19], provided by experts in the field.” Published in March 2020 and updated as recently as August 2020, the article has received more than 660,000 interactions to date on Facebook and other social media platforms according to the social media analytics tool CrowdTangle. Some of the top sharers of the article include Facebook groups that oppose vaccination and groups like QAnon that promote conspiracy theories. Health Feedback examined some of the claims made in the article, listed below.
Claim 1:
“According to the latest immunological studies, the overall lethality of Covid-19 (IFR) is about 0.1% to 0.3% and thus in the range of a severe influenza (flu).”
The claim is inaccurate. The overall infection fatality rate (IFR) is defined as the proportion of deaths among all infected people. The overall IFR for flu has been estimated at 0.04%, according to this Twitter thread by Christophe Fraser, an epidemiologist at Oxford University, while the U.S. Centers for Disease Control and Prevention’s (CDC) current best estimate for the overall IFR of COVID-19 is 0.65%. This value is based on a systematic review and meta-analysis of 24 studies, including serological surveys[1], although the authors cautioned that variations in age and underlying co-morbidities in a population could mean that different regions observe different IFRs. The most recently updated estimates in this preprint (a study that has not been peer-reviewed yet) indicate that the overall IFR could span a range of values between 0.53 to 0.82%. Based on this data, the listicle of “facts about COVID-19” underestimates COVID-19’s overall IFR.
In addition, many more deaths have occurred this year than expected, based on the mortality levels seen in previous years. This is known as excess mortality. The New York Times has reported that at least 200,000 excess deaths have occurred in the U.S. since March 2020. Notably, the level of excess mortality in 2020 exceeds the level observed during the 2017-2018 flu pandemic, which was considered to be a severe flu season in the U.S. and Europe (Figures 1 and 2). This strongly indicates that the COVID-19 mortality rate is higher than that of a severe flu season.
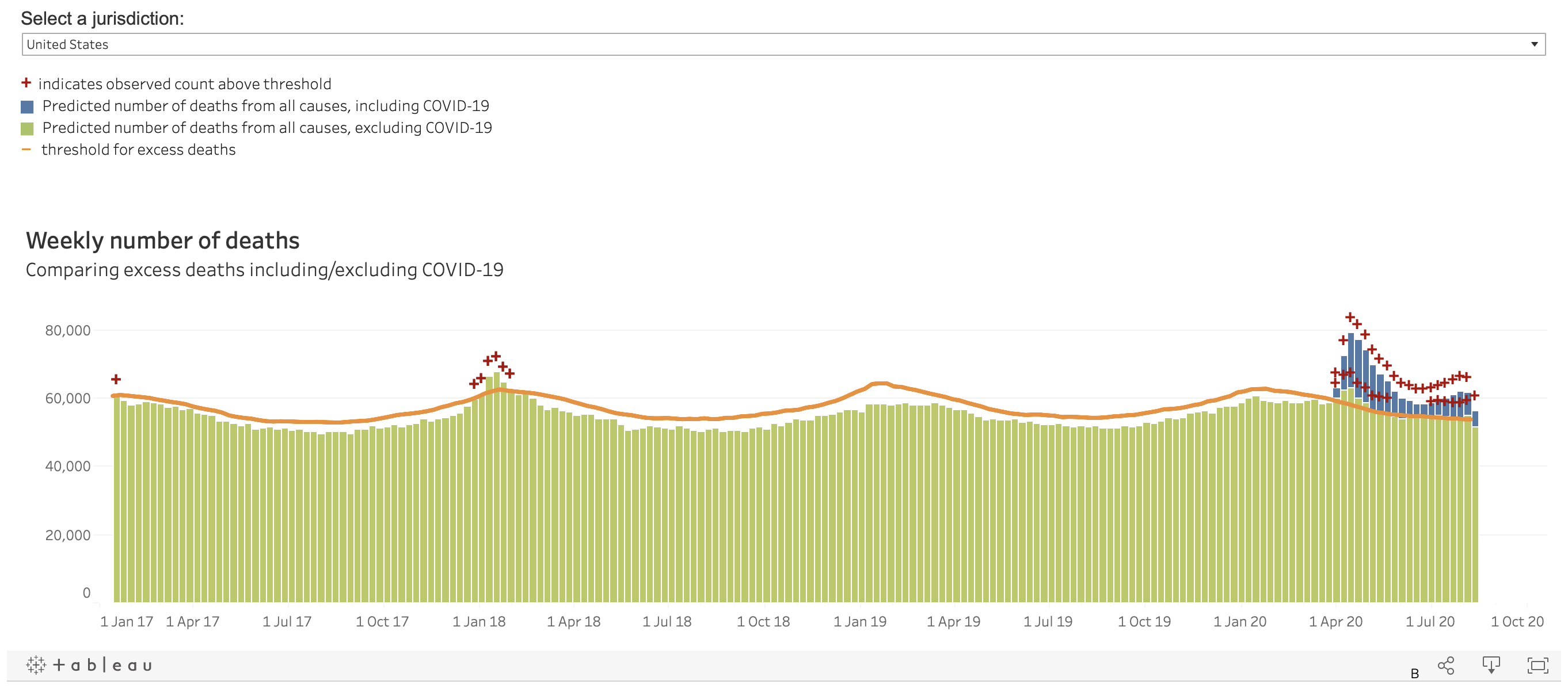
Figure 1. Weekly excess mortality levels from all causes in the U.S. between 2017 and 2020. Note the excess deaths (bars above the threshold in orange) observed early in 2018 as a result of the flu season. Data from the U.S. Centers for Disease Control and Prevention (CDC) (extracted on 25 August 2020).
The European Mortality Monitoring Project (EuroMOMO), a collaborative project involving the European Centre for Disease Prevention and Control, the World Health Organization, and the Statens Serum Institute in Denmark, tracks excess mortality across 24 European countries. As shown in Figure 2, there was a spike in mortality in early 2020 that greatly exceeded mortality trends observed from 2016 through 2019. For example, the 2020 peak represents more than double the number of excess deaths (almost 35,000) compared to the next highest peak observed in early 2017 (about 15,000 excess deaths). This pattern of higher excess deaths in 2020 also occurred in non-European countries, as detailed in this Economist report.
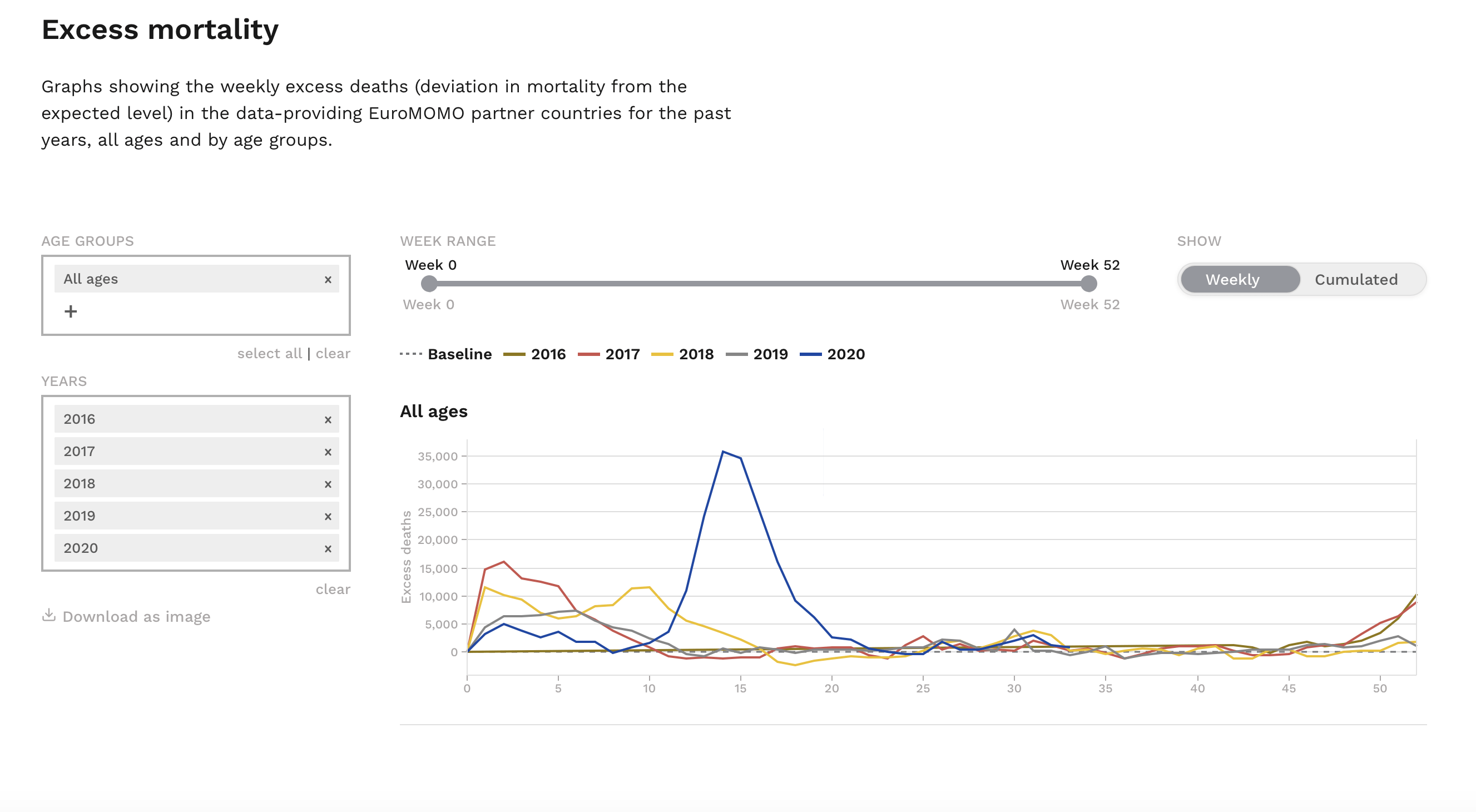
Figure 2. Weekly excess mortality levels between 2016 and 2020 from 24 participating European countries. Data from EuroMOMO (obtained on 25 August 2020).
Claim 2:
“Up to 60% of all persons may already have a certain cellular background immunity to the new coronavirus due to contact with previous coronaviruses (i.e. cold viruses). The initial assumption that there was no immunity against the new coronavirus was not correct.”
This claim is inaccurate and unsupported. The claim is based on a Cell study by Griford et al., which detected a certain type of immune cells, called memory T cells, that are capable of recognizing a variety of proteins on SARS-CoV-2, the virus that causes COVID-19, in people who had not previously been exposed to it[2]. Another study discovered that these cells were generated through infection with coronaviruses that cause the common cold[3]. These findings suggest that memory T cells might play a role in the immune response against SARS-CoV-2 infection.
However, scientists have not established whether the presence of memory T cells is associated with protection from COVID-19, although this is the subject of ongoing research. Therefore, the article’s suggestion that more than half of the population is already immune to SARS-CoV-2 is unsupported. Health Feedback explored the potential implications of memory T cells in COVID-19 immunity in detail in a previous article review.
Shane Crotty, an immunologist and professor at the La Jolla Institute for Immunology, who co-authored the Cell study cited above, debunked the claim about pre-existing immunity in the following Twitter thread:
1/ There are various tweets misinterpreting COVID-19 “pre-existing immunity” and making dangerous claims about herd immunity. Since many of those claims refer to our scientific papers, we will reiterate the facts. @SetteLab @ljiresearch @ScienceMagazine @CellCellPress pic.twitter.com/gCZwFMW1iU
— Shane Crotty (@profshanecrotty) August 12, 2020
Claim 3:
“Countries without lockdowns, such as Japan, South Korea, Belarus, and Sweden, have not experienced a more negative course of events than many other countries. Sweden was even praised by the WHO and now benefits from higher immunity compared to lockdown countries. 75% of Swedish deaths happened in nursing facilities that weren’t protected fast enough.”
Sweden, Belarus, and Japan did not implement lockdowns, but this is not the case for South Korea, which implemented lockdown measures in August 2020 following a rising number of COVID-19 cases. It is worth noting that the pre-existing cultural norms in three of these countries (Japan, South Korea, and Sweden) led the majority of people to voluntarily practice physical distancing. For instance, Sweden’s chief epidemiologist, Anders Tegnell, stated that Swedes reduced their social interactions to 30% of pre-pandemic levels, and the Swedish Civil Contingencies Agency reported that about 87% of people followed physical distancing recommendations, according to a July 2020 BBC report.
In contrast to Western countries, the practice of mask-wearing during a disease outbreak is a cultural norm in East Asian countries like Japan and South Korea, which may have also mitigated disease transmission independent of a lockdown.
Given the differences in adherence to public health recommendations as a result of cultural differences between countries, it is extremely difficult to determine whether outcomes of COVID-19 differ across countries solely as a result of whether lockdowns were implemented. The suggestion that lockdowns do not work was also refuted in a previous Health Feedback review.
Claim 4:
“There is still little to no scientific evidence for the effectiveness of cloth face masks in healthy and asymptomatic individuals. Experts warn that such masks may interfere with normal breathing and may become “germ carriers” if used repeatedly.”
This claim is mostly inaccurate and misleading. Scientific studies on the effectiveness of face mask use in the community were scarce in the early days of the COVID-19 pandemic, and guidance regarding their use was mixed. However, there is now a growing body of scientific evidence suggesting that wearing a mask is better than having no protection at all. This Health Feedback review discusses the numerous studies demonstrating that face masks can be helpful for reducing virus transmission.
On 5 June 2020, the World Health Organization (WHO) updated its interim guidance on the use of masks by the public based on increasing evidence supporting the effectiveness of wearing face masks. Mask use was not initially encouraged by the WHO during the early stage of the pandemic, but the guidance now reads:
“[T]aking into account the available studies evaluating pre-[symptomatic] and asymptomatic transmission, a growing compendium of observational evidence on the use of masks by the general public in several countries, individual values and preferences, as well as the difficulty of physical distancing in many contexts, WHO has updated its guidance to advise that to prevent COVID-19 transmission effectively in areas of community transmission, governments should encourage the general public to wear masks in specific situations and settings as part of a comprehensive approach to suppress SARS-CoV-2 transmission.”
However, it is true that cloth face masks can be an infection risk if people fail to handle them correctly or wash them properly, hence health authorities like the CDC have recommended that people regularly wash their cloth face masks and their hands after handling a used mask.
Claim 5:
“The virus test kits used internationally are prone to errors and can produce false positive and false negative results. Moreover, the official virus test was not clinically validated due to time pressure and may sometimes react positive to other common coronaviruses.”
The accuracy of a diagnostic test for COVID-19 is determined by its sensitivity and specificity. As this article in The Conversation explains:
“A sensitive test will correctly identify people with the disease. Sensitivity measures correct positive results.
If a test is 90% sensitive, it will correctly identify 90% of people who are infected – called a true positive. However, 10% of people who are infected and tested would get a false negative result – they have the virus, but the test said they don’t.
A specific test will accurately identify people without the disease. Specificity measures correct negatives.
If a test is 90% specific, it will correctly identify 90% of people who are not infected – registering a true negative. However, 10% of people who are not infected will test positive for the virus and receive a false positive.
To reiterate: Sensitivity measures positive accuracy; specificity measures negative accuracy.”
It is important to keep in mind that there is no diagnostic test with 100% accuracy, that is, 100% specificity and 100% sensitivity. Therefore all diagnostic tests, including tests for COVID-19, are capable of producing false-positive and false-negative results.
SARS-CoV-2 infection can be detected in two ways. One is the RT-PCR method, which detects the genetic material of the virus and is considered the gold standard for SARS-CoV-2 detection. As such, RT-PCR is the method of choice for detecting a current SARS-CoV-2 infection in most countries. However, the test is prone to false negatives, which can arise due to issues with sample collection, storage conditions, and handling. This means that the test may erroneously inform infected people that they do not have the infection. However, RT-PCR testing for SARS-CoV-2 is highly specific for the virus and does not react to other coronaviruses, such as those that cause the common cold, because the test is based on unique sequences in the viral genome. This is explained in greater detail in this Health Feedback review.
Another method used to detect SARS-CoV-2 infection is antibody or serological testing, which can tell us the number of people in a given population who were once infected and allows for estimates of the spread of the disease. However, the test is not useful for detecting a current infection and is also prone to false positives, as the presence of antibodies against other coronaviruses besides SARS-CoV-2 can produce a positive result. Furthermore, some studies suggest that antibodies produced in response to an infection with SARS-CoV-2 may not be long-lasting[4,5], therefore antibody tests may also miss detecting a prior infection.
It is not clear what the article means by “the official virus test”, although the source it provides for the claim is a YouTube video of an interview with German physician Wolfgang Wodarg, produced by a group that has voiced support for conspiracy theories about the pandemic, as documented in this Undark article. The German fact-checking organization Correctiv has also fact-checked Wodarg’s claims in the video and found them to be inaccurate and unsubstantiated.
Claim 6:
“Numerous internationally renowned experts in the fields of virology, immunology, and epidemiology consider the measures taken to be counterproductive and recommend rapid natural immunization of the general population and protection of risk groups.”
The claim is based on several articles by OffGuardian, labeled a conspiracy website by Media Bias/Fact Check, which cherry-picked quotes from various scientists that purportedly show that lockdowns and physical distancing are counterproductive for managing the COVID-19 pandemic. However, on closer examination, none of the quotes provide any scientific evidence supporting these claims, even though several scientists expressed concerns about the economic and psychological impacts of lockdowns.
A June 2020 study published in Nature by Flaxman et al. found that non-pharmaceutical interventions in 11 European countries, including physical distancing, school closures, and national lockdowns in particular, were effective at reducing the transmission of COVID-19[6]. Another Nature study published by a research group at the University of California, Berkeley, analyzed the effects of physical distancing and lockdowns in Asia, Europe, and the U.S. on COVID-19, and also found that these interventions helped reduce disease transmission[7].
The approach of allowing “natural” herd immunity to develop in a population was considered in some countries, but the World Health Organization warned that this would lead to many preventable deaths. Although the overall IFR of COVID-19 is currently estimated to be 0.65%, which some have considered “low”, this can still translate to a few million deaths as two epidemiologists pointed out in a New York Times opinion article. Furthermore, not all COVID-19 patients recover fully; scientists have observed that the damage from the infection can lead to potentially long-term complications.
REFERENCES
- 1 – Meyerowitz-Katz and Merone. (2020) A systematic review and meta-analysis of published research data on COVID-19 infection-fatality rates. medRxiv.
- 2 – Grifoni et al. (2020) Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell.
- 3 – Mateus et al. (2020) Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans. Science.
- 4 – Long et al. (2020) Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nature Medicine.
- 5 – Ibarrondo et al. (2020) Rapid Decay of Anti–SARS-CoV-2 Antibodies in Persons with Mild Covid-19. New England Journal of Medicine.
- 6 – Flaxman et al. (2020) Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature.
- 7 – Hsiang et al. (2020) The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature.


