
Introduction
The World Health Organization considers access to safe and affordable abortion services as important for the good health and well-being of women and girls. Unsafe abortion methods contribute to a significant portion of maternal deaths, and this is particularly evident in places where abortion is legally restricted. However, the development of medical abortion, a non-invasive method which doesn’t require training, has helped to reduce deaths and injuries associated with unsafe abortion, by increasing the safety of self-induced abortion[1].
A medical abortion, also known as medication abortion, is a procedure that involves the use of medications to end a pregnancy. This procedure doesn’t require surgery, as opposed to surgical abortion, and can be performed up to around nine weeks of pregnancy. Medical abortion usually involves taking two different medications one after the other, mifepristone and misoprostol.
Mifepristone, taken first, blocks the hormone progesterone. This hormone prepares the tissue lining of the womb to allow implantation of the fertilized egg, and prevents contractions during pregnancy, which could lead to a miscarriage. Mifepristone prepares the uterus for the effect of the second medication used in medical abortion, misoprostol.
Misoprostol, usually taken 24 to 48 hours after mifepristone, causes the uterus to contract and ends the pregnancy. While misoprostol alone can be used to end a pregnancy, using it with mifepristone is less likely to cause incomplete abortions, and is associated with fewer side effects[2].
Currently, mifepristone accounts for more than half of all abortions performed in the U.S., as reported by this article from the Guttmacher Institute, a non-profit organization that advocates for sexual and reproductive health.
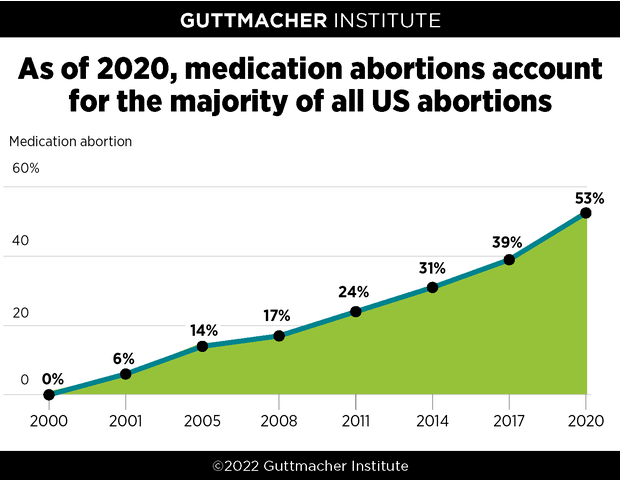
Figure 1. Proportion of medical abortions to the total number of abortions since mifepristone was legalized in the U.S. in 2000. Source: Guttmacher Institute.
The U.S. Food and Drug Administration (FDA) has approved the use of mifepristone in a regimen with misoprostol to terminate pregnancy during the first ten weeks of gestation. Initially mifepristone could only be offered in clinics and hospitals, but as of 3 January 2023, the FDA also allows mifepristone to be dispensed by certified pharmacies. Misoprostol is already available in pharmacies, since it is also used for other purposes besides medical abortion, such as preventing gastric ulcers.
Following this change in regulation that would increase access to safe and effective abortion, online posts have circulated questioning the safety of mifepristone, or promoting the scientifically unsupported procedure called abortion reversal.
Mifepristone is considered a safe abortion method during the early stage of pregnancy
The safety of medical abortion has been the subject of strong assertions, such as in this LifeNews article claiming that mifepristone poses a threat to women’s health and describing it as “the dangerous abortion drug that has […] injured thousands of women”. LifeSite is owned by the Conservative Campaign Life Coalition, an advocacy group which campaigns against abortion, among other issues.
One piece of evidence used to support this assertion was an FDA report on post-marketing adverse events of mifepristone in the U.S., which allegedly “linked mifepristone to at least 26 women’s deaths and 4,000 serious complications between 2000 and 2018”. However, the FDA report itself stated that “fatal cases are included regardless of causal attribution to mifepristone”. This means that a causal relationship between mifepristone and these deaths wasn’t actually established.
Another piece of evidence the LifeNews article cited to support the claim that mifepristone is dangerous was a study by the Charlotte Lozier Institute, an anti-abortion organization, which reported an increase in the rate of abortion-related emergency room visits by women taking mifepristone compared to women who underwent a surgical abortion[3].
The study included 423,000 induced abortions, both medical and surgical, performed in the U.S. between the years 1999 and 2015, and 121,283 emergency room visits occurring within 30 days of the procedure. The LifeNews article claimed that “abortion-related emergency room visits by women taking [mifepristone] increased more than 500 percent between 2002 and 2015”. The study reported that emergency room visits following medical abortion with mifepristone grew from 3.6% of all abortion-related visits in 2002 to 33.9% of all abortion-related visits in 2015.
However, the study also reported an increase in the proportion of abortions performed by medical means from 4.4% of total abortions in 2002 to 34.1% in 2015. Therefore, the framing of the study as evidence of mifepristone’s danger is premature, as the increase in the ratio of emergency room visits in women who underwent medical abortion with mifepristone could simply reflect an increase in the ratio of medical abortions, over the same time period.
The study also comes with important limitations. One of these is that the reasons for the women’s emergency room visits weren’t specified. Emergency room visits were classified as “abortion-related” according to the International Classification of Diseases, a standard used for diagnostic purposes.
However, health conditions in this category include, among others, molar pregnancy, an unusual growth of cells due to atypical fertilization of the egg, and ectopic pregnancy, consisting of the implantation of the fertilized egg outside the uterus. These conditions result in a miscarriage, but aren’t known to be caused by medical abortion. Mifepristone is contraindicated in cases of ectopic pregnancy, as the symptoms experienced after a medical abortion (abdominal pain, uterine bleeding) are similar to those of a ruptured ectopic pregnancy, a life-threatening condition.
As the authors of the study didn’t specify what the reasons for the emergency room visits were, it isn’t possible to establish whether the visits were causally related to medical abortion in the first place. Another limitation is that the study also didn’t examine how serious these women’s conditions were, for instance, by examining whether the women needed hospitalization.
Overall, the study doesn’t provide enough information to reliably determine whether the increase in the rate of emergency room visits following medical abortion is actually a reflection on the safety of medical abortion, or whether it’s simply a reflection of the increase in the number of medical abortions being done.
The study is now under investigation by the journal for “potential issues regarding the representation of data in the article and author conflicts of interest”, according to an Expression of Concern issued on 25 July 2023.
This investigation was launched after South University pharmaceutical sciences professor Chris Adkins contacted the journal in April 2023 to express concerns over the methodology of the study, as well as how the findings were reported, Colorado Newsline reported in August 2023. He pointed out that “the study doesn’t actually show […] that medication abortion leads to significantly high rates of complications”. However, the data in the study were presented in various misleading ways to suggest otherwise, leading Adkins to call it “dishonest science”.
Some of the study’s deficiencies that Adkins and other researchers highlighted are the following:
- In the emergency visits analyzed by the study, the researchers didn’t distinguish between routine medical care and adverse events. The codes used to capture these visits “lump in issues like ectopic and molar pregnancies, which are medical emergencies not necessarily related to having taken abortion drugs”.
- The findings were consistent with healthcare developments during the time period analyzed in the study: increased use of medication abortion and the rise in the number of Medicare patients following the Affordable Care Act. “What they find is exactly what you would expect to find when you expand coverage and expand care,” Adkins told States Newsroom.
- The researchers didn’t provide an estimated total of emergency department visits among Medicaid patients to contextualize the number of abortion-related visits they estimated in the study. Suzanne Bell, a professor at Johns Hopkins Bloomberg School of Public Health told States Newsroom that “I imagine the 790 ER visits they identified as associated with a recent medication abortion is a very small percentage of the total number of ER visits and in no way would risk overwhelming the medical system”.
Another issue with the study is the fact that the authors declared “no potential conflict of interest with respect to the research”, but also stated that the study was funded by the anti-abortion Charlotte Lozier Institute. Five of the eight authors of the study, including the principal investigator, were also affiliated with the Charlotte Lozier Institute.
Specifically, the study’s lead researcher, James Studnicki, is vice president and director of data analysis at the Charlotte Lozier Institute. Another co-author of the study is a member of the American Association of Pro-Life Obstetricians and Gynecologists, another anti-abortion organization. Altogether, the affiliations of several of the study authors and their failure to disclose their conflict of interest raise questions about transparency and potential bias in the interpretation of their findings.
Another study was cited by LifeSite as reporting that “as many as one in 17 women [required] hospital treatment” following medical abortion[4]. The study, conducted in Finland, did a follow-up of 42,619 women who underwent induced abortion between 2000 and 2006, both medical (22,368 women) and surgical (20,251 women).
The study included records of adverse events for which women sought hospital treatment within 42 days after termination of pregnancy. The study reported that the incidence of adverse events was higher after medical abortion (20%) compared with surgical abortion (5.6%). The authors concluded that “[b]oth methods of abortion are generally safe, but medical [abortion] is associated with a higher incidence of adverse events”, mainly hemorrhage (15.6%) and incomplete abortion (6.7%).
A year after the study was published, several gynecologists addressed a letter to the editor, pointing out that “other databases and peer-reviewed literature about medical abortion report a dramatically lower incidence of complications” than the earlier study[5].
In response to the letter, the authors of the original study explained that “many of the ‘complications’ are not really such, but rather concerns or adverse events that bring women back to the health care system”. The authors noted that the results were “reassuring” regarding the safety of medical abortion, as the “rate of serious, ‘real’ complications is rare and rather similar between surgical and medical abortion”.
Therefore, in light of this clarification by the study authors and the additional information provided by other gynecologists in the letter to the editor, LifeSite’s citation of the study as showing that “the risks are more common than what abortion activists often claim” is highly misleading.
In a comment to Health Feedback, Jonathan Lord, a consultant gynecologist and spokesperson for the Royal College of Obstetricians and Gynecologists (RCOG), said “Mifepristone is recommended as a safe option for abortion by the World Health Organisation. Medical and surgical abortions are safe procedures for which major complications are uncommon at any stage of pregnancy. Whilst any procedure does carry some risk, the vast majority of medical abortions occur without any complications” [See below for the full comment by the RCOG.].
There are scientific studies showing that mifepristone is safe and effective for abortion. A study in the U.S., funded by Planned Parenthood which provides contraception and abortion services, followed more than 13,300 women for 63 days after using mifepristone and misoprostol, reporting an efficacy of 97.7%[6]. The authors reported that hospitalization following medical abortion was rare, reporting two cases due to infection (incidence of 0.01%) and four due to hemorrhage requiring transfusion (0.03%). They concluded that their findings “reinforces the safety and efficacy of the evidence-based regimen for medical abortion”.
Another study led by Marie Stopes, a non-governmental organization providing contraception and abortion services, included more than 13,000 women in Australia who followed the same procedure with mifepristone and misoprostol. The study reported an efficacy of 95.16%[7].
Among the roughly 11,000 women who were available to follow-up, 674 serious adverse events following medical abortion were reported, including 633 cases of incomplete abortion requiring surgical intervention (4.84%), 15 cases of infection (0.11%) and 17 cases of hemorrhage requiring transfusion (0.13%). The researchers concluded that the regimen was highly effective and had a “favourable safety profile”, although the relatively large number of women who couldn’t be reached for follow-up meant that accurately determining the complete abortion rate wasn’t possible.
A study conducted in Norway included more than 1,000 women who sought medical abortion up to 63 days of pregnancy to evaluate the safety of medical abortion using mifepristone and misoprostol at home[8]. The study reported a rate of complete abortion of 93.6%, with 4.9% of cases requiring surgical evacuation. Moderate to severe pain was experienced by 68.4% of the participants, and 74.7% reported moderate to severe bleeding. The authors concluded that the use of mifepristone and misoprostol is safe and effective.
No reliable evidence supports using progesterone for abortion reversal
Apart from spreading misinformation about mifepristone’s safety, some online content have gone a step further to promote the concept of “abortion reversal”, such as these articles which were published after the FDA changed mifepristone regulations.
Abortion reversal is considered the “brainchild” of George Delgado, a family medicine physician and researcher affiliated with anti-abortion organizations. He is the medical director of Abortion Pill Reversal, an anti-abortion organization that advocates using progesterone for abortion reversal. Delgado has previously claimed without evidence that induced abortion increases the risk of breast cancer and mental illness.
Abortion reversal involves taking doses of progesterone within 24 to 72 hours after taking mifepristone. The idea is to reverse the effect of mifepristone, which blocks progesterone.
Delgado was the lead author of an observational study often cited to provide scientific evidence for the claim that medical abortion can be reversed using progesterone[9]. However, it’s important to note that the study, involving a case series report of 754 patients on varying regimens of progesterone, included no control group (a group that didn’t receive progesterone). Curiously, the study was published in Issues in Law & Medicine, which isn’t a medical or scientific journal but rather focuses on medical law.
In this case series report, the authors reported that intramuscular progesterone had a 64% abortion reversal rate, while oral progesterone had a 68% abortion reversal rate. The authors concluded that progesterone is effective at reversing the effects of mifepristone by comparing these results to “a control mifepristone embryo survival rate, derived from the literature”, which was 25%.
An inspection of the references shows that this figure comes from an earlier review co-authored by Delgado and also published in Issues in Law & Medicine[10], and is the upper limit of a range of survival rates derived from multiple earlier studies. It’s questionable whether this figure serves as a reliable control group to that of the progesterone-treated groups, since we don’t know how similar or different the women from previous studies are to the groups in Delgado’s study.
Professional medical organizations have pointed out that using progesterone to reverse abortion isn’t supported by scientific evidence. A joint statement by RCOG, the Faculty of Sexual and Reproductive Healthcare, the Royal College of Midwives, and the British Society of Abortion Care Providers clarified that there is no evidence that progesterone treatment increases the likelihood of continuing pregnancy after taking mifepristone, and specifically advised against administering progesterone.
Regarding the safety of progesterone administration after the use of mifepristone, the RCOG states:
“Although progesterone is a commonly used medication for other reasons (such as period control or as part of IVF), it does commonly cause side effects and is expensive. Those that prescribe it following mifepristone use very high doses, and without any evidence of benefit it means the only effects are negative ones such as bowel disturbance, bloating and mood disorder.”
The American College of Obstetricians and Gynecologists (ACOG) also warns that the use of progesterone as a treatment to reverse abortion is not supported by scientific evidence, describing this procedure as “unproven and unethical”, and warning about the dangers to women’s health of “legislative mandates based on unproven and unethical research”.
The ACOG notes that most of the evidence for abortion reversal treatments is based on case series reports, which don’t prove that progesterone administration was the cause for continuation of pregnancy, as they lack appropriate control groups. The organization emphasizes that “case series with no control groups are among the weakest forms of medical evidence”, and raises concerns about the ethics and scientific validity of the results of such studies.
A systematic review on abortion reversal found no evidence that taking progesterone after taking mifepristone increased the likelihood of continuation of pregnancy compared to taking mifepristone alone[11].
Only a single study on medical abortion reversal met the inclusion criteria for the review. Notably, this was a study co-authored by Delgado, which performed a follow-up of six patients, four of which continued the pregnancy and delivered at term, and two others that aborted within three days of taking mifepristone[12].
However, the review reported that the study was of poor quality, with unclear inclusion criteria, no control group, and the study authors didn’t specify the amount of progesterone that the women received. The study also didn’t report how many women seeking medical abortion reversal after taking mifepristone were found to have already aborted and were excluded from treatment. As the review explained, this is important information:
“In order to calculate the proportion of women with a continuing pregnancy seeking this treatment, which would be comparable to the proportion of continuing pregnancies after mifepristone alone, one must know how many women requested treatment and were found to already have an embryonic demise or incomplete abortion.”
Despite its significant methodological weaknesses, this study has been used by anti-abortion physicians to promote progesterone for abortion reversal.
The review also examined 13 studies about continuing pregnancy following administration of mifepristone alone. These studies reported that the proportion of pregnancies continuing up to two weeks after using mifepristone ranged from 8 to 46%. In other words, taking mifepristone alone in itself can result in continued pregnancy, even without taking progesterone.
The authors of the review noted that continuation of pregnancy was more frequent with lower doses of mifepristone and advanced gestational age at the time of medication use. They concluded that recommendations on the use of medication after taking mifepristone to ensure continuation of pregnancy is “scientifically untenable”, as there is “no credible evidence” that using progesterone after taking mifepristone is better than taking mifepristone alone in assuring a continued pregnancy.
Conclusion
Reliable scientific evidence indicates that using mifepristone and misoprostol for medical abortion is effective and safe, with complications requiring hospital care being rare. Criticisms of the safety of mifepristone, which can commonly be traced back to anti-abortion advocacy groups, are unfounded and based on cherry-picked and misinterpreted studies. To date, the procedure known as abortion reversal, which involves administering progesterone after a woman has already taken mifepristone, isn’t supported by reliable scientific evidence, as progesterone hasn’t been shown to increase the likelihood of continuation of pregnancy any more than taking mifepristone alone would.
The Royal College of Obstetricians and Gynecologists:
Mifepristone is the first medication used within a medical abortion, and can also [be] used to prepare the womb before a surgical abortion. It works as a priming agent so that the next set of drugs, misoprostol, work more effectively to cause the womb to contract and expel the pregnancy.
Mifepristone is recommended as a safe option for abortion by the World Health Organisation. Medical and surgical abortions are safe procedures for which major complications are uncommon at any stage of pregnancy. Whilst any procedure does carry some risk, the vast majority of medical abortions occur without any complications.
Abortion aftercare will vary in each country. In the UK system (the NHS), most patients who need after care can do so through their abortion provider using scheduled appointments, and all patients have access to 24 hour aftercare advice lines. Almost all complications from abortion can be managed through planned care, and attendance at the accident and emergency department is very rarely needed.
UPDATE (9 August 2023):
This article was updated to reflect recent developments regarding the study by Studnicki et al., which is now currently under investigation by the journal for issues regarding the way it represented data and for conflicts of interest, according to an August 2023 report by Colorado Newsline. This information can be found in the seventeenth to the twenty-second paragraphs.
REFERENCES
- 1 – Zamberlin et al. (2012) Latin American women’s experiences with medical abortion in settings where abortion is legally restricted. Reproductive Health.
- 2 – World Health Organization (2014) Clinical practice handbook for safe abortion
- 3 – Studnicki et al. (2021) A Longitudinal Cohort Study of Emergency Room Utilization Following Mifepristone Chemical and Surgical Abortions, 1999–2015. Health Services Research and Managerial Epidemiology.
- 4 – Niinimäki et al. (2009) Immediate complications after medical compared with surgical termination of pregnancy. Obstetrics and Gynecology.
- 5 – Fjerstad et al. (2010) Immediate Complications After Medical Compared With Surgical Termination of Pregnancy. Obstetrics and Gynecology.
- 6 – Gatter et al. (2016) Efficacy and safety of medical abortion using mifepristone and buccal misoprostol through 63 days. Contraception.
- 7 – Goldstone et al. (2017) Efficacy and safety of mifepristone–buccal misoprostol for early medical abortion in an Australian clinical setting. Australian and New Zealand Journal of Obstetrics and Gynaecology.
- 8 – Løkeland et al. (2014) Medical abortion with mifepristone and home administration of misoprostol up to 63 days’ gestation. Acta Obstetricia et Gynecologica Scandinavica.
- 9 – Delgado et al. (2018) A case series detailing the successful reversal of the effects of mifepristone using progesterone. Issues in Law & Medicine.
- 10 – Davenport et al. (2017) Embryo Survival after Mifepristone: A Systematic Review of the Literature. Issues in Law & Medicine.
- 11 – Grossman et al. (2015) Continuing pregnancy after mifepristone and “reversal” of first-trimester medical abortion: a systematic review. Contraception.
- 12 – Delgado and Davenport (2012) Progesterone use to reverse the effects of mifepristone. Annals of Pharmacotherapy.
