
Inadequate support: There is no clinical evidence supporting the use of vitamin B as a cure for Hashimoto’s disease.

FULL CLAIM: There is nothing wrong with the thyroid in patients with Hashimoto’s disease ; Hashimoto’s disease is “diagnosed as clinically low T3” whereas only 20% of T3 comes from the thyroid; Hashimoto’s disease is “a fancy way of pushing thyroid medication”; vitamin B is a cure for Hashimoto’s disease
REVIEW
In July 2024, health influencer Gary Brecka criticized the standard diagnosis and treatment of the autoimmune disorder Hashimoto’s disease.
In a Facebook reel that generated more than 200,000 views at the time of writing, Brecka declared that the way Hashimoto’s disease is explained to patients is “nonsense” and is only “a fancy way of pushing thyroid medication”. He claimed that there is “nothing wrong” with the thyroid of patients with Hashimoto’s disease and that vitamin B is a cure for the disease.
There is a lot to unpack in Brecka’s claim and we explain below why most of his assertions are inaccurate. To understand why, we first need to briefly explain what thyroid hormones are.
The thyroid produces the metabolism-regulating hormones T3 and T4
The thyroid is part of the body’s endocrine system. It’s a gland located in the neck that responds to signals from the brain called thyroid-stimulating hormone, or TSH. The thyroid secretes hormones that control body functions such as metabolism, heart rate, and body temperature. In children, thyroid hormones are also important for brain development.
When the thyroid doesn’t produce enough hormones, it may lead to a condition called hypothyroidism. This is characterized by symptoms including fatigue, soreness, weight gain, dry skin, intolerance to cold, and constipation. By contrast, excessive production of hormones is called hyperthyroidism. Some of its symptoms are the opposite of hypothyroidism, such as intolerance to heat, weight loss, and diarrhea.
Two of the hormones secreted by the thyroid are called T4 (thyroxine) and T3 (triiodothyronine). The thyroid mostly produces T4 and only small amounts of T3, but the secreted T4 is subsequently converted into T3 in other tissues. Cells are unresponsive to T4 and more sensitive to T3, so we can see T4 as a biologically inactive precursor of T3.
Only 20% of T3 directly comes from the thyroid; the rest comes from converting T4 to T3. But a key point to remember is that T4 is also produced in the thyroid. So, all T3 originates from the thyroid, either directly or indirectly.
Hashimoto’s disease is a thyroid disorder, resulting in thyroid hormone deficiency
Hashimoto’s disease is rather common, affecting about five in 100 people in the U.S. The disease progresses slowly, so people may remain asymptomatic for a while. When symptoms appear, patients may develop a goiter or enlarged thyroid. At a later stage, patients may show symptoms of hypothyroidism.
Brecka claimed that Hashimoto’s disease isn’t a thyroid problem because it’s defined by “clinically low T3” and the thyroid is responsible for producing only a fifth of T3. In other words, Brecka claims the thyroid only contributes to a relatively small amount of T3 in the body, so it cannot be the main cause of low T3 levels. Instead, low T3 could only be explained by another defect that doesn’t involve the thyroid.
But this claim is flawed for two reasons.
First, Hashimoto’s disease does affect the thyroid. Hashimoto’s disease is an autoimmune disease in which the patient’s immune system attacks their own thyroid. This usually happens because the immune system produces antibodies against a protein called thyroid peroxidase (TPO) that is important for the thyroid to function.
Some white blood cells called lymphocytes may also infiltrate the thyroid and cause inflammation (thyroiditis). For that reason, Hashimoto’s disease is also known as chronic lymphocytic thyroiditis. Over time, this process damages the thyroid gland and impairs its ability to produce hormones.
Science Feedback reached out to experts for comment [See scientists’ full comments here]. Victor Bernet, an endocrinologist at the Mayo Clinic, explained the sequence of hormonal imbalances during the course of the disease: “A rise in thyroid stimulating hormone (TSH) will be the first sign that the thyroid is slowing down. Free T4 levels will be the next to drop.”
Regina Castro, another endocrinologist at the Mayo Clinic, confirmed that Hashimoto’s disease “is generally associated with elevated levels of serum thyroid stimulating hormone (TSH), low levels of thyroxine, and elevated levels of TPO antibodies”.
Second, Brecka is also wrong in claiming that Hashimoto’s disease is defined as “low T3”.
Instead, the telltale signs of Hashimoto’s disease are high levels of TSH, low levels of T4, and/or anti-TPO antibodies, as detailed by the Cleveland Clinic. Blood levels of T3 are typically not used to diagnose Hashimoto’s disease.
As Bernet explains:
“T3 levels, whether free or total, are not considered very reliable assays particularly for the diagnosis of hypothyroidism. […] Reduction in T3 levels is one of the last things to happen with primary hypothyroidism. Of note, all three major medical societies—the American Thyroid Association, Endocrine Society, and AACE—all recommend against using T3 levels for the diagnosis and/or management of patients with hypothyroidism.”
Castro concurred with this idea, stating that “low T3, especially if also associated with low T4, may be seen in patients with thyroid dysfunction, but it is not generally the main test used to diagnose thyroid dysfunction”.
As Bernet explained, a low level of T3 may occur but it is only a potential late stage effect symptom:
“A drop in T3 is the last to happen as the body will continue to convert available T4 into T3 using deiodinase enzymes present in various tissues.”
In other words, just because only 20% of T3 directly originates from the thyroid doesn’t mean the thyroid isn’t the root problem in Hashimoto’s. The rest of T3 is converted from T4, which is produced in the thyroid. If the thyroid cannot produce T4, it makes sense that it eventually leads to lower levels of T3 as well.
In summary, Brecka presented an inaccurate description of Hashimoto’s disease. Contrary to his claim, Hashimoto’s is an autoimmune disorder that affects the thyroid and impairs its hormone production. A low level of T3 isn’t the primary criterion for diagnosing Hashimoto’s disease.
There’s no evidence that vitamin B is a cure for Hashimoto’s disease
Brecka claimed that Hashimoto’s disease comes from a problem in converting T4 to T3 via a chemical reaction called methylation. He also proposed that vitamin B could solve this problem by inducing methylation, thereby curing Hashimoto’s. This is incorrect.
The hormone T4 is converted into T3 through deiodination, not methylation. Deiodination and methylation are two different processes. Deiodination is a chemical reaction that removes an atom of iodine from a molecule[1], whereas methylation is a reaction that adds a methyl group made of carbon and hydrogen to a molecule.
Figure 1 below illustrates the transformation of T4 into T3. As we can see, no methyl group is added, and instead one atom of iodine is removed.
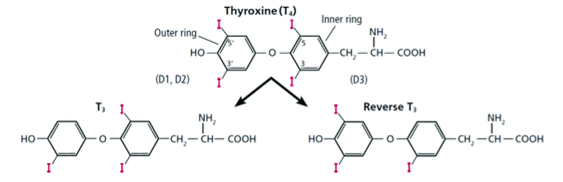
Figure 1 – Conversion of T4 into T3. The molecular structures of the T4 and T3 hormones, as well as another thyroid hormone called reverse T3. Iodine atoms are represented in magenta. Note that the removal of one iodine atom from the outer ring of T4 turns it into T3. The reaction is catalyzed by the enzymes D1 and D2. Source: Gomes-Lima et al.[2].
Moreover, there is no clinical data indicating that vitamin B is able to cure Hashimoto’s disease.
Instead, the proven treatment for Hashimoto’s is a hormone replacement therapy using a synthetic form of T4 called levothyroxine, which Castro described as “very safe and effective”. This makes sense because, as we explained above, Hashimoto’s disease impairs the thyroid’s ability to produce T4.
Conclusion
Hashimoto’s disease is an autoimmune disorder where the immune system attacks the thyroid, causing inflammation. It can eventually impair thyroid hormone secretion and lead to hypothyroidism. Brecka’s claim that there is no problem with the thyroid in patients with Hashimoto’s disease is thus in direct contradiction with medical facts.
A low level of T3 may occur at a later stage of Hashimoto’s disease as a consequence of the thyroid’s impaired ability to produce it or its precursor T4. That said, a low level of T3 isn’t the main criterion for diagnosis of Hashimoto’s disease, contrary to Brecka’s claim.
Finally, Brecka’s claim that vitamin B is an alternative treatment for Hashimoto’s isn’t supported by clinical evidence. Instead, the proven treatment involves replacement hormones such as levothyroxine to compensate for the loss of T4 production in the thyroid.
SCIENTISTS’ FEEDBACK
Victor Bernet, Professor of Medicine, Mayo Clinic:
Hashimoto’s thyroiditis, also known as chronic lymphocytic thyroiditis, is an autoimmune condition that can increase the risk of thyroid dysfunction, particularly development of hypothyroidism (under-function of the thyroid). However, some people with Hashimoto’s thyroiditis can maintain normal thyroid function for years or even decades. Therefore, Hashimoto’s thyroiditis does not equate to having hypothyroidism, [although] many with Hashimoto’s thyroiditis may develop hypothyroidism over time.
Assuming normal pituitary function, a rise in thyroid stimulating hormone (TSH) will be the first sign that the thyroid is slowing down. Free T4 levels will be the next to drop. A drop in T3 is the last to happen as the body will continue to convert available T4 into T3 using deiodinase enzymes present in various tissues.
T3 levels, whether free or total, are not considered very reliable assays particularly for the diagnosis of hypothyroidism. As noted above, reduced T3 levels is one of the last things to happen with primary hypothyroidism. Of note, all three major medical societies—the American Thyroid Association, Endocrine Society, and the American Association of Clinical Endocrinology—recommend against using T3 levels for the diagnosis and/or management of patients with hypothyroidism.
If one has hypothyroidism then there is an underproduction of thyroid hormone. The most common treatment for hypothyroidism is therapy with levothyroxine (LT4) which is a thyroid hormone using either brand or generic formulations to get thyroid hormone levels back to physiologic levels. We focus on getting the TSH, the sensitive pituitary signal, back into the appropriate range, usually around a goal of 1 to 3 μIU/ml [IU: International Units].
Occasionally, patients are treated with a combination of T4 and T3 (liothyronine), but experience indicates the majority of patients do well with just T4 alone. There are also desiccated animal thyroid hormone products (e.g. Armour, Nature Thyroid) which contain both T4 and T3, but not in a ratio consistent with typical human physiology. That being said, some patients seem to prefer this type of therapy. Many thyroid specialists are not fans of this type therapy as it can be problematic to dose accurately over time.
Vitamin B is not a treatment for hypothyroidism.
Regina Castro, Professor of Medicine, Mayo Clinic:
The statement that Hashimoto’s disease is “diagnosed as clinically low T3” is inaccurate.Hashimotos’ disease is an autoimmune disorder of the thyroid in which antibodies directed against thyroid cells (TPO) result in chronic inflammation and [can lead to] to hypothyroidism.
It is generally associated with elevated levels of serum thyroid stimulating hormone (TSH), low levels of thyroxine, and elevated levels of TPO antibodies. Some patients may have only elevated levels of TSH with normal T4 levels early in the course of the disease (a stage called subclinical hypothyroidism).
Low T3, especially if also associated with low T4, may be seen in patients with thyroid dysfunction, but low T3 is not generally the main test used to diagnose thyroid dysfunction.
There is no evidence that vitamin B is helpful for Hashimoto’s disease. It is false to claim that levothyroxine should be avoided. Levothyroxine is the standard of care for the treatment of hypothyroidism associated with Hashimoto’s thyroiditis and is very safe and effective.
REFERENCES
- 1 – St Germain et al. (2009) Defining the Roles of the Iodothyronine Deiodinases: Current Concepts and Challenges. Endocrinology.
- 2 – Gomes-Lima et al. (2019) Can Reverse T3 Assay Be Employed to Guide T4 vs. T4/T3 Therapy in Hypothyroidism? Frontiers in Endocrinology.


