Misleading: A rising incidence of melanoma, particularly in Europe and North America, isn’t caused by sunscreen. It’s instead linked to modifiable risk factors like excessive unprotected sun exposure and the use of tanning beds. There’s a lack of evidence supporting the implication that low vitamin D is causally associated with melanoma.

FULL CLAIM: “So we got sunlight for millions of years and we're totally fine. Sunscreen was invented in the 1930s and then all of a sudden melanoma started skyrocketing in the 1950s. Melanoma is associated with low vitamin D. But it's the sun's fault? Make it make sense please.”
REVIEW
A Facebook reel published in early November 2024 claimed that “we got sunlight for millions of years and we’re totally fine”, but once sunscreen was invented, melanoma began skyrocketing. It also implied that sun exposure doesn’t cause melanoma and that low vitamin D is causally linked to melanoma risk.
The reel, which was viewed more than 420,000 times, was posted by the Facebook page Eraofhealth, which has more than 216,000 followers. A similar post on Instagram by the account @carnivoreaurelius from August 2024 also made the same claim.
The reel repeats the common but false claims that sun exposure is unrelated to skin cancer and that sunscreen causes skin cancer. Science Feedback debunked these claims in earlier reviews.
Our findings in previous reviews showed that the causal relationship between excessive sun exposure and skin cancer and the biological mechanism behind this relationship are well-established. Sunlight contains UV radiation, a known cancer-causing agent. UV radiation can cause DNA damage, which can produce mutations that trigger cancerous transformation in cells. Scientific evidence indicates that using sunscreen reduces the risk of skin cancer[1-3].
Rise in melanoma incidence isn’t causally linked to sunscreen
Melanoma is a type of skin cancer that starts in melanocytes, the cells in our skin that produce melanin. Melanin is responsible for skin color and pigmentation. Exposure to UV radiation, like during sunbathing, triggers the production of more melanin. This is why skin tends to darken after prolonged exposure to sunlight. Melanoma is considered a more dangerous form of skin cancer, because it is more likely to spread to other parts of the body if not found and treated early.
Melanoma is particularly prevalent in regions of the world with a greater proportion of white people. A 2024 report by the International Agency for Cancer Research indicates that Europe and North America combined accounted for almost 80% of new melanoma cases in 2022. In contrast, melanoma incidence in Asia was about 8%, while in Africa it was about 2%.
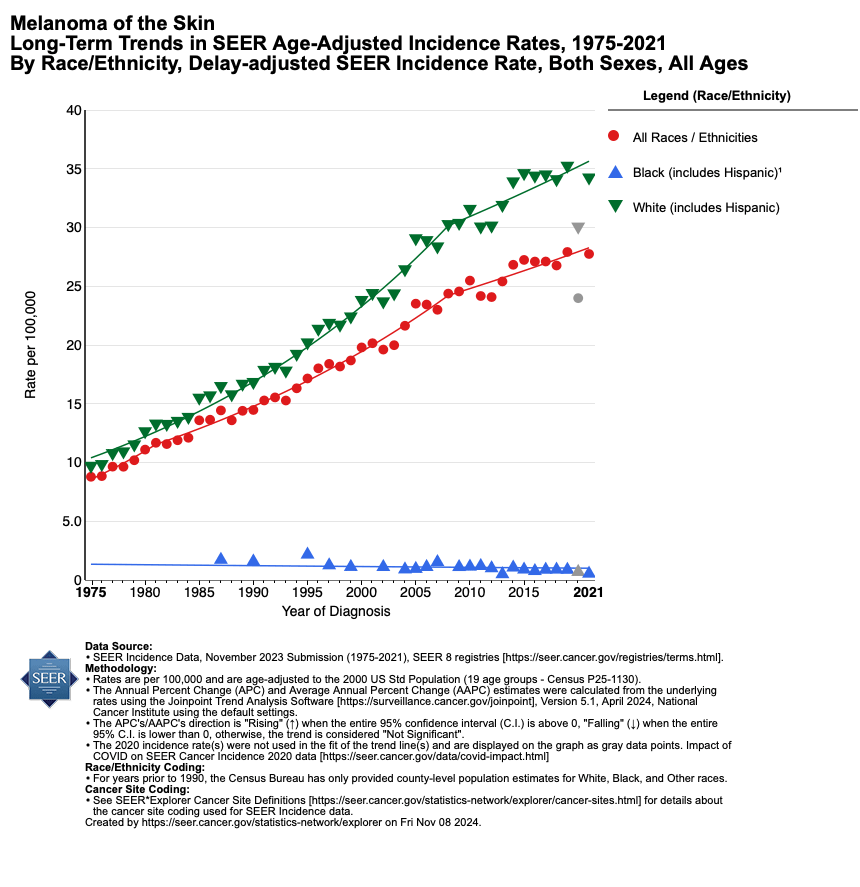
Figure 1 — Age-adjusted melanoma incidence rates in the U.S. from 1975 to 2021. Incidence for all races/ethnicities is indicated in red, for Black people in blue, and for White people in green. Source: Surveillance, Epidemiology, and End Results Program, U.S. National Cancer Institute.
Part of the greater incidence in predominantly white populations has to do with sunburn risk. People with white or fair skin tend to burn more easily when exposed to sunlight, and getting sunburned increases the risk of skin cancer. The Skin Cancer Foundation states that just “one blistering sunburn in childhood or adolescence more than doubles your chances of developing melanoma later in life”. The American Cancer Society (ACS) states that “Overall, the lifetime risk of getting melanoma is about 3% (1 in 33) for White people, 0.1% (1 in 1,000) for Black people, and 0.5% (1 in 200) for Hispanic people”.
The reel’s implication that melanoma is a novel phenomenon that only began to appear after sunscreen was invented is false. A brief timeline of sunscreen development showed that an early form of sunscreen was developed in the late 1890s, while the first modern sunscreen was developed by Swiss chemist Franz Greiter in the late 1940s. But the earliest description of melanoma can be found in the writings of Hippocrates, who lived between 460 to 375 BCE. And French physician René Laennec lectured on melanoma in the 1800s.
It’s true that the incidence of melanoma has indeed risen over time (see Figure 1 above) and has correlated with sunscreen use. Scientists have coined the term “sunscreen paradox” to describe this phenomenon.
However, this isn’t because sunscreen is intrinsically cancer-causing. Instead, some findings suggest that wearing sunscreen provides people with a false sense of security, leading them to spend longer periods under the sun than they would have without sunscreen[4,5].
Another reason for the rise in melanoma incidence is a rising proportion of elderly people in the population, as a risk factor for melanoma is age.
However, melanoma is also common in young people. In fact, the ACS states that it’s one of the most common cancers in those under 30, especially young women.
One likely contributor to this trend is tanning culture, based on the popular association of tanned skin with health and beauty in Western countries. This perception promotes behaviors that increase one’s risk of melanoma, such as excessive unprotected sun exposure and use of tanning beds[6].
The American Academy of Dermatology states that “Using tanning beds before age 20 can increase your chances of developing melanoma by 47%, and the risk increases with each use”. It also states that the majority of melanoma cases can be attributed to UV exposure.
Overall, the reel’s implications that sun exposure is unrelated to melanoma and that sunscreen is responsible for melanoma are false and soundly refuted by scientific evidence. Excessive exposure to sunlight increases the amount of DNA damage caused by UV radiation from the sun, which raises the risk of mutations that can lead to cancer like melanoma.
Sunscreen helps reduce the damage caused by UV radiation. However, it’s not 100% protective against UV radiation. Experts recommend that people take multiple measures in addition to wearing sunscreen in order to reduce UV exposure, such as wearing sun-protective clothing and reducing or avoiding time spent in the sun.
Evidence that vitamin D influences the risk of melanoma is preliminary
The reel’s statement that “melanoma is associated with low vitamin D” may mislead users into thinking that low vitamin D could cause melanoma. However, this interpretation isn’t currently substantiated by scientific evidence.
Vitamin D is a fat-soluble substance that’s essential to health. It’s important for calcium absorption, making it essential for building and maintaining strong bones. It also regulates the level of calcium and phosphate ions in the blood, which affects muscle contraction, and helps the immune system work properly.
Our body makes vitamin D through exposure to sunlight. UV radiation in sunlight jumpstarts the cascade of chemical reactions that produces vitamin D in the body. However, as we explained earlier, too much exposure to UV radiation increases our risk of skin cancer like melanoma.
Another way we can obtain vitamin D is through our diet. Fatty fish like salmon and mackerel and fortified foods like milk and yogurt are naturally rich in vitamin D. Vitamin D supplements are also a way to obtain sufficient vitamin D.
The reel’s statement on vitamin D is based on this meta-analysis from 2023 (a full copy of the study can be found here). To assess the relationship between melanoma and vitamin D insufficiency, the authors analyzed eight published studies that compared vitamin D levels in the blood of healthy people and in those with cutaneous melanoma (a form of melanoma that appears on the skin). The authors reported that those with melanoma were more likely to have vitamin D insufficiency, defined as vitamin D levels below 20 nanograms/deciliter (ng/dl).
However, association alone isn’t sufficient evidence of causality. Indeed, the authors concluded by stating that the “data suggests that vitamin D insufficiency is significantly associated with a higher incidence of [cutaneous melanoma]”, but that this evidence was of “low quality” and with “moderate risk of bias”.
Moreover, several of the studies analyzed in the meta-analysis compared healthy people with people who’d already been diagnosed with melanoma (case-control studies). These studies didn’t have data on the vitamin D status of melanoma patients before they were diagnosed with melanoma.
This data is important, as cancer doesn’t develop overnight. To better determine if low vitamin D levels are linked to an increased melanoma risk, we would also need to track people’s vitamin D levels before melanoma is diagnosed.
It’s also important to be aware that a person’s vitamin D level can be influenced by their health status. For example, difficulty absorbing nutrients and lack of sunlight can contribute to low vitamin D levels. Those in poorer health, like cancer patients, may be more likely to have these risk factors. People who’ve been diagnosed with melanoma are particularly advised to minimize their exposure to the sun.
Because of these caveats affecting the meta-analysis, we can’t rely on it to establish that the observed tendency for lower vitamin D levels in melanoma patients is a cause of the melanoma. Indeed, it’s possible that the lower vitamin D levels are simply a consequence of the disease.
According to the U.S. National Cancer Institute (NCI), some data suggests that higher vitamin D levels are associated with reduced risk of colorectal cancer and bladder cancer, and that overall cancer mortality tends to be greater in those with low vitamin D levels. But in the case of breast and lung cancer, no association between cancer risk and vitamin D levels has been established. The NCI also states that most randomized clinical trials found that taking vitamin D supplements “do[es] not reduce the risk of developing cancer overall or of developing specific cancers”.
The nonprofit Cancer Research UK states that “There isn’t enough convincing evidence to link low levels of vitamin D (vitamin D deficiency) to cancer. And there’s not evidence to support taking vitamin D supplements to reduce cancer risk”.
Overall, scientific evidence shows that having sufficient vitamin D is essential to health. Some studies have found correlations between low vitamin D levels and poorer cancer outcomes. However, there’s currently no reliable evidence showing that vitamin D supplementation can ward off cancer or improve cancer outcomes. Further research in this area is still needed.
Conclusion
The causal relationship between excessive sun exposure and skin cancer and the biological mechanism behind this relationship are well-established. UV radiation in sunlight is a known cancer-causing agent. UV radiation can cause DNA damage, which can produce mutations that lead to cancer. Scientific evidence indicates that using sunscreen reduces damage from UV radiation and thus the risk of skin cancer. While having sufficient vitamin D is essential to health, it’s still unclear whether vitamin D levels directly affect melanoma risk. Additional research is needed to shed more light on this question.
REFERENCES
- 1 – Watts et al. (2018) Sunscreen Use and Melanoma Risk Among Young Australian Adults. JAMA Dermatology.
- 2 – Green et al. (1999) Daily sunscreen application and betacarotene supplementation in prevention of basal-cell and squamous-cell carcinomas of the skin: a randomised controlled trial. The Lancet.
- 3 – Gordon et al. (2020) Prevention versus early detection for long-term control of melanoma and keratinocyte carcinomas: a cost-effectiveness modelling study. BMJ Open.
- 4 – Alli et al. (2023) Understanding the Perceived Relationship between Sun Exposure and Melanoma in Atlantic Canada: A Consensual Qualitative Study Highlighting a “Sunscreen Paradox”. Cancers.
- 5 – Jeremian et al. (2023) Gene–Environment Analyses in a UK Biobank Skin Cancer Cohort Identifies Important SNPs in DNA Repair Genes That May Help Prognosticate Disease Risk. Cancer Epidemiology, Biomarkers & Prevention.
- 6 – Wehner et al. (2014) International Prevalence of Indoor Tanning: A Systematic Review and Meta-analysis. JAMA Dermatology.