Unsupported: Large clinical trials show no evidence of memory loss, dementia, or Alzheimer’s in people taking cholesterol-lowering drugs for many years.
Incorrect: The cause of Alzheimer’s is unknown. Although the disease damages nerve myelin, it is unclear whether this is a consequence of neuronal damage or contributes to it. The brain produces its own cholesterol; it is still unknown whether and how dietary cholesterol affects brain metabolism.
FULL CLAIM: “Alzheimer’s disease did not occur 40 years ago”; “They give you cholesterol-lowering drugs. Then you can't remember who you are. You’re going to have Alzheimer’s disease now, because you can't rebuild the myelin in the brain”
REVIEW
A Facebook reel claiming “Drs. Cause Alzheimers [sic]” went viral in mid-March 2023, receiving more than 113,000 views. The video featured a speech by veterinarian and naturopath Joel Wallach, who claimed that Alzheimer’s is a new disease that “did not occur 40 years ago” and is caused by “a cholesterol-restricted diet” and “cholesterol-lowering drugs”.
The video originated from a TikTok account that contained more videos of Wallach and sold dietary supplements from Youngevity, a brand founded by Wallach.
But the claim that Alzheimer’s is a new condition caused by lowering cholesterol levels in the blood with diet or medication is incorrect and contradicts current scientific evidence about the role of cholesterol in Alzheimer’s, as we will explain below.
Alzheimer’s disease was first described over a century ago
Wallach’s claim that Alzheimer’s “did not occur 40 years ago, even by another name” is outright false. Alzheimer’s disease is the main cause of dementia, a general term that refers to the impaired ability to remember, think, or make decisions up to the point of interfering with the person’s daily life. The concept of dementia has been documented since ancient history, but because the condition is linked to aging, the number of cases has increased with increasing human lifespan.
In 1906, German pathologist Alois Alzheimer described the first case of Alzheimer’s in the 37th Meeting of South-West German Psychiatrists held in Tuebingen, Germany. Alzheimer reported the case of a 51-year-old woman with an “Unusual Illness of the Cerebral Cortex” that caused memory loss, aggressiveness, disorientation, and delusions[1].
The autopsy revealed that the woman’s brain cortex, which is the brain’s outer layer, was thinner than usual and had abnormal deposits called senile plaques outside the neurons. These plaques had been observed before in the elderly but not in younger people. Using a new silver stain, Alzheimer could also identify the presence of twisted fibers (tangles) inside the neurons for the first time.
Alzheimer’s discovery didn’t draw much attention at that time. But after other physicians started to report similar cases, psychiatrist Emil Kraepelin introduced the term “Alzheimer’s disease” to refer to the condition in the 1910 edition of his Compendium of Psychiatry.
Later research showed that the plaques and tangles that Alzheimer identified are the hallmarks of Alzheimer’s disease, and they result from an abnormal accumulation of the proteins amyloid-beta and tau outside (amyloid-beta plaques) and inside (neurofibrillary tangles) neurons (Figure 1). However, it is still unknown whether these changes are a cause of the disease or a result of it.
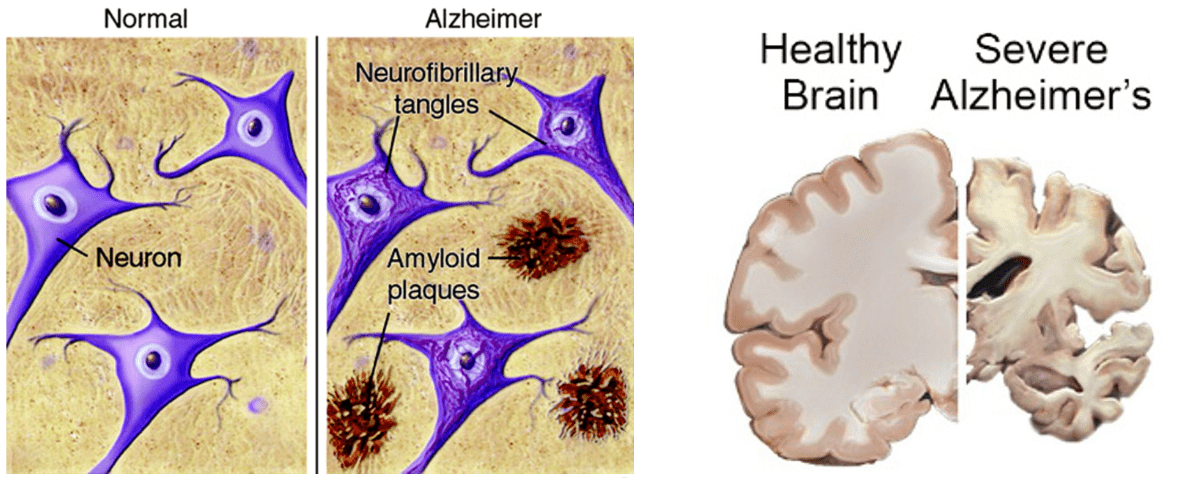
Figure 1. Left, representation of amyloid-beta plaques and neurofibrillary tangles in the brain of a healthy person and a person with Alzheimer’s disease[3]. Right, widespread brain damage and shrinking in the brain of a deceased Alzheimer’s patient. Source: U.S. National Institute of Aging.
Therefore, contrary to Wallach’s claim, Alzheimer’s disease isn’t new but was described long before cholesterol-lowering drugs entered the market around the mid-1960s[2].
Large clinical trials haven’t found an association between cholesterol-lowering drugs and a higher risk of cognitive problems
In 2012, the U.S. Food and Drug Administration (FDA) updated the safety label for the cholesterol-lowering drugs statins to include potential cognitive side effects. This update followed rare reports of “memory loss and confusion” in some people taking statins. Although the FDA clarified that these events “were generally not serious and went away once the drug was no longer being taken”, the update led to concerns that statins might increase the risk of dementia and Alzheimer’s disease.
However, the American Heart Association published a scientific statement in 2019 saying that there is no evidence of a causal link between effects such as forgetfulness and confusion and statin use[4]. The statement also pointed out that “Complaints such as these are common in middle-aged and older people, regardless of whether or not they are treated with a statin”, and therefore, randomized clinical trials are required to demonstrate a causal link.
It’s worth noting that large clinical trials evaluating cognitive function in people using statins[5] and other cholesterol-lowering medications[6] to reduce their risk of heart attacks and strokes haven’t found such an association.
In 2002, the PROSPER (Prospective Study of Pravastatin in the Elderly at Risk)[7] trial and the U.K. Heart Protection Study[8] assessed the frequency of cognitive effects in more than 25,000 participants aged 40 to 82 years with a high risk of coronary disease in Scotland, Ireland, the Netherlands, and the U.K. None of the studies found differences in cognitive function between the participants who used statins for three and five years respectively and those who didn’t use statins.
In 2014, the Statin Safety Assessment Task Force convened by the U.S. National Lipid Association published an assessment of the effects of statins on cognitive function based on the evidence available at that time[9]. The panel concluded that “although cognitive side effects of statins may occur in rare individuals, the medical evidence supporting a causal effect is weak or nonexistent”.
Later observational studies also found no association between the use of statins and cognitive problems, including Alzheimer’s[9,10]. For example, one large study published in the Journal of the American College of Cardiology in 2021 analyzed data from the 18,846 participants in the ASPREE (ASPirin in Reducing Events in the Elderly) trial, which included people aged 65 and older from Australia and the U.S[11]. The researchers found no difference in the risk of dementia and Alzheimer’s nor changes in memory, language, behavior, and psychomotor speed between the participants who used statins for almost five years and those who didn’t.
High cholesterol levels might increase the risk of Alzheimer’s disease
Contrary to Wallach’s suggestion that a cholesterol-rich diet would prevent Alzheimer’s, a growing body of evidence suggests that high levels of cholesterol in the blood might increase the risk of developing dementia and Alzheimer’s later in life[12].
Based on this association, some researchers hypothesized that by lowering cholesterol levels, statins might reduce the risk of developing dementia. Indeed, some studies have observed an association between statin use and a lower risk of cognitive problems, including Alzheimer’s and dementia in general. However, studies evaluating this hypothesis have produced mixed results.
For example, a 2013 analysis by Swiger and colleagues pooled data from eight clinical trials including over 23,000 participants with a high risk of cardiovascular disease who had been taking statins for three to 25 years[13]. The researchers found that those taking statins had a 29% lower risk of developing dementia later in life compared to those who didn’t take statins.
Later analyses, including trials as well as observational studies, reported similar risk reductions in dementia, Alzheimer’s disease, and mild cognitive problems in people using statins compared to those who didn’t[14-17].
One study found a similar association between statin use and a lower risk of dementia in people who had suffered a traumatic brain injury, a condition that increases the risk of cognitive problems[18].
In contrast to these studies suggesting a potential benefit of statins in preventing cognitive problems, statin use didn’t show an association with cognitive improvements in people who already had an established mild to moderate Alzheimer’s[19]. Furthermore, not all studies have shown a benefit from statin use on cognitive function[20-22]. One reason for these conflicting results is that most of the available evidence on statin use and cognitive protection comes from observational studies. This type of study can be subject to bias and confounding factors, making it difficult to detect a causal association.
For example, people with high cholesterol levels often have additional risk factors for cognitive problems and Alzheimer’s, such as high blood pressure and diabetes. In addition, research shows that statins have other effects unrelated to cholesterol metabolism, including beneficial effects on blood vessels, oxidative stress and inflammation, and immune function[23], some of which might influence cognitive function independently of cholesterol levels. Therefore, evaluating the potential benefit of statins in cognitive function will require more research involving robust clinical trials.
Our understanding of the relationship between cholesterol levels in blood, cholesterol processing in the brain, myelin damage, and Alzheimer’s is still evolving
Wallach claimed that the cause of Alzheimer’s is that “you can’t rebuild the myelin in the brain”. Specifically, he claimed that myelin is “100% cholesterol” and when you take cholesterol-lowering drugs, “you don’t have enough raw materials to replace” the myelin that is lost. This claim is incorrect for several reasons.
Firstly, evidence shows that Alzheimer’s harms myelin—a protective sheath that wraps around some nerves—and the cells responsible for producing it, the oligodendrocytes[24]. It also shows that cholesterol metabolism most likely plays a role in this process[25]. But the cause of Alzheimer’s remains unknown to date, despite Wallach claiming otherwise. Researchers know that the affected neurons stop working correctly, lose connections with other neurons, and ultimately die, but they haven’t identified the underlying cause of this process.
Secondly, although cholesterol is the most abundant component of myelin, it isn’t the only one as Wallach claimed. Myelin contains at least 70% of fats, of which cholesterol accounts for approximately half (35% of the total myelin components). The remaining 20 to 30% of myelin components are proteins. However, the fact that cholesterol is the main component of nerve myelin doesn’t necessarily imply that there is a correlation between the amount of cholesterol in myelin nerves and cholesterol levels in blood.
It is important to note that cholesterol itself can’t cross the blood-brain barrier (BBB), a network of blood vessels and tissue that protects the brain. Instead, the brain produces its own cholesterol and has specific mechanisms for regulating its cholesterol metabolism[26]. Therefore, the brain doesn’t depend on dietary cholesterol to produce myelin. Outside the brain, the liver produces most of the cholesterol that the body needs, and only around 20% of it comes through food from animal sources such as egg yolks, meat, and dairy products.
Nevertheless, one product of cholesterol metabolism, 27-Hydroxycholesterol, does cross the BBB and has been associated with effects on cognitive function. In 2021, one small trial showed that lifestyle changes that reduced the blood levels of this metabolite improved cognitive performance, particularly memory, in people aged 60 to 77 years at a high risk of cardiovascular disease[27]. However, the trial had a small number of participants. Also, it is possible that the lifestyle interventions caused changes in other factors apart from the metabolite that could have influenced the observed effects.
In summary, our understanding of the role of cholesterol and myelin damage in Alzheimer’s is still evolving. But Wallach’s claim that lowering cholesterol levels through diet or medication damages myelin and causes Alzheimer’s is unsupported and reflects a misunderstanding of how cholesterol is produced and regulated in the brain.
Conclusion
The claim that Alzheimer’s is a new disease that didn’t exist four decades ago and is caused by low-cholesterol diets and cholesterol-lowering medications is inaccurate and contradicts current scientific evidence. Symptoms of dementia have been reported early in history. Specifically, the term Alzheimer’s disease to describe a particular type of dementia was introduced more than a century ago.
Contrary to the claim, large clinical trials haven’t found evidence of an association between statins and other cholesterol-lowering medications and cognitive problems, dementia, and Alzheimer’s. On the contrary, high cholesterol levels in the blood are associated with a higher risk of developing dementia and Alzheimer’s. In fact, some studies suggest that statins might help decrease the risk of developing these conditions later in life.
REFERENCES
- 1 – Stelzmann et al. (1995) An English Translation of Alzheimer’s 1907 Paper, “Über eine eigenartige Erlranliung der Hirnrinde”. Clinical Anatomy.
- 2 – Endo (2010) A historical perspective on the discovery of statins. Proceedings of the Japan Academy.
- 3 – Silbert (2007) Does statin use decrease the amount of Alzheimer disease pathology in the brain? Neurology.
- 4 – Newsman et al. (2015) Statin Safety and Associated Adverse Events: A Scientific Statement From the American Heart Association. Arteriosclerosis, Thrombosis, and Vascular Biology.
- 5 – Ott et al. (2015) Do Statins Impair Cognition? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of General Internal Medicine.
- 6 – Janik et al. (2021) Alirocumab treatment and neurocognitive function according to the CANTAB scale in patients at increased cardiovascular risk: A prospective, randomized, placebo-controlled study. Artherosclerosis.
- 7 – Shepherd et al. (2002) Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. The Lancet.
- 8 – Heart Protection Study Collaborative Group (2002) MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: a randomised placebocontrolled trial. The Lancet.
- 9 – Rojas-Fernandez et al. (2014) An assessment by the Statin Cognitive Safety Task Force: 2014 update. Journal of Clinical Lipidology.
- 10 – Richardson et al. (2013) Statins and Cognitive Function. A Systematic Review. Annals of Internal Medicine.
- 11 – Zhou et al. (2021) Effect of Statin Therapy on Cognitive Decline and Incident Dementia in Older Adults. Journal of the American College of Cardiology.
- 12 – Zhang et al. (2022) Midlife lipid and glucose levels are associated with Alzheimer’s disease. Alzheimer’s and Dementia.
- 13 – Swiger et al. (2013) Statins and Cognition: A Systematic Review and Meta-analysis of Short- and Long-term Cognitive Effects. Mayo Clinic Proceedings.
- 14 – Chu et al. (2018) Use of statins and the risk of dementia and mild cognitive impairment: A systematic review and meta-analysis. Scientific Reports.
- 15 – Poly et al. (2020) Association between Use of Statin and Risk of Dementia: A Meta-Analysis of Observational Studies. Neuroepidemiology.
- 16 – Olmastroni et al. (2021) Statin use and risk of dementia or Alzheimer’s disease: a systematic review and meta-analysis of observational studies. European Journal of Preventive Cardiology.
- 17 – Macedo et al. (2014) Unintended effects of statins from observational studies in the general population: systematic review and meta-analysis. BMC Medicine.
- 18 – Redelmeier et al. (2019) Association Between Statin Use and Risk of Dementia After a Concussion. JAMA Neurology.
- 19 – Feldman et al. (2010) Randomized controlled trial of atorvastatin in mild to moderate Alzheimer disease. LEADe. Neurology.
- 20 – McGuiness et al. (2016) Statins for the prevention of dementia. Cochrane Database of Systematic Reviews.
- 21 – Power et al. (2015) Statins, cognition, and dementia—systematic review and methodological commentary. Nature Reviews Neurology.
- 22 – Mielke et al. (2005) High total cholesterol levels in late life associated with a reduced risk of dementia. Neurology.
- 23 – Liao & Laufs (2005) Pleiotropics Effects of Statins. Annual Review of Pharmacology and Toxicology.
- 24 – Nasrabady et al. (2018) White matter changes in Alzheimer’s disease: a focus on myelin and oligodendrocytes. Acta Neuropathologica Communications.
- 25 – Blanchard et al. (2022) APOE4 impairs myelination via cholesterol dysregulation in oligodendrocytes. Nature.
- 26 – Zhang & Liu (2015) Cholesterol metabolism and homeostasis in the brain. Protein and Cell.
- 27 – Sandebring-Matton et al. (2021) 27-Hydroxycholesterol, cognition, and brain imaging markers in the FINGER randomized controlled trial. Alzheimer’s Research and Therapy.