Factually inaccurate: Multiple scientific studies and population-level analyses have established that vaccinated people are less likely to die from COVID-19 compared to unvaccinated people.
FULL CLAIM: Higher COVID-19 vaccination rates in White people are related to higher COVID-19 death rates
REVIEW
Entrepreneur and podcaster David Harris Jr. posted a picture on Instagram of headlines from two news articles, one from CNN in January 2021, and the other from the Washington Post in October 2022, with the caption “Just posting two headlines from Wapo that I’m sure have nothing to do with each other…” The picture was credited to Newsmax host Carl Higbie.
Higbie’s post of the image, also on Instagram, received approximately 4,100 likes, but Harris’ share of the image received more than 42,000 likes within a day of posting.
Both Higbie and Harris have previously posted COVID-19 misinformation. Higbie claimed people have a “99% chance of surviving COVID” (incorrect) and that people who aren’t sick don’t have COVID-19 (many infected people aren’t sick initially but are still contagious during the incubation period). Harris claimed the COVID-19 vaccine killed more children than it saved (this is false) and implied ivermectin is an effective COVID-19 treatment (there’s no reliable evidence for this claim).
The Instagram posts run in the same vein. The image, by juxtaposing two headlines about the higher COVID-19 vaccination rate and a rise in COVID-19 mortality in White people, implied that there was a causal relationship between the two. Comments left under these posts also show that the posts were interpreted in that manner. One user stated “So glad I opted out of the ‘depopulation’ plandemic. Not jabbed, never scared, didn’t die”. Another commented: “I’m white and unvaxxed. Saw through the lies and sham right away”.
However, the implication made in the posts is simply not consistent with the evidence.
Evidence shows COVID-19 vaccination reduces COVID-19 mortality risk
Multiple scientific studies have established that getting vaccinated against COVID-19 reduces the risk of dying from COVID-19[1-5].
Population-level data from different countries compiled and analyzed by Our World in Data are also consistent with the findings in these studies, showing higher COVID-19 mortality rates in the unvaccinated, not the vaccinated (see Figures 1, 2 and 3 below).
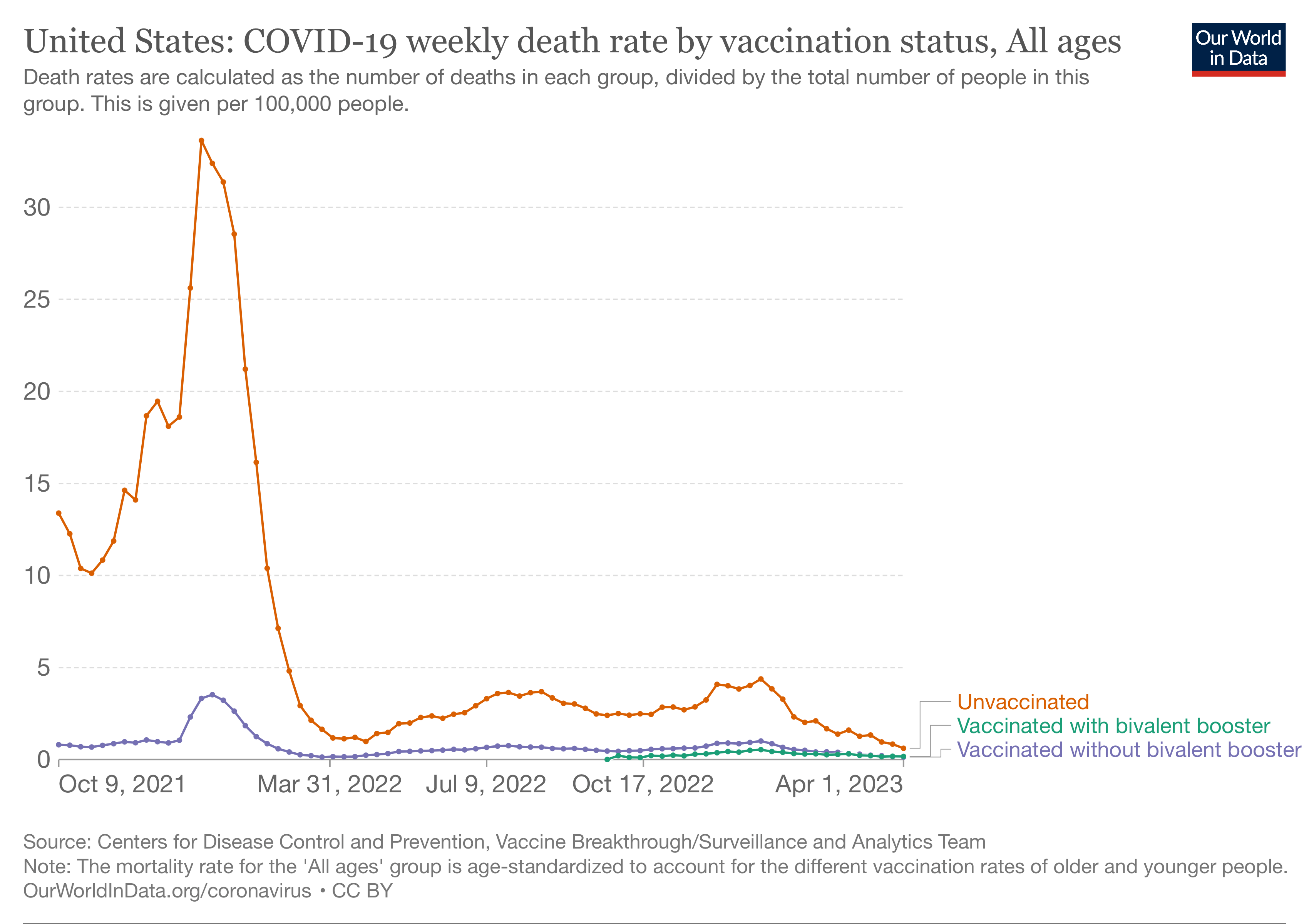
Figure 1. The U.S. COVID-19 weekly age-standardized mortality rate (per 100,000 people) based on vaccination status. Chart from Our World in Data. Retrieved on 24 August 2023.
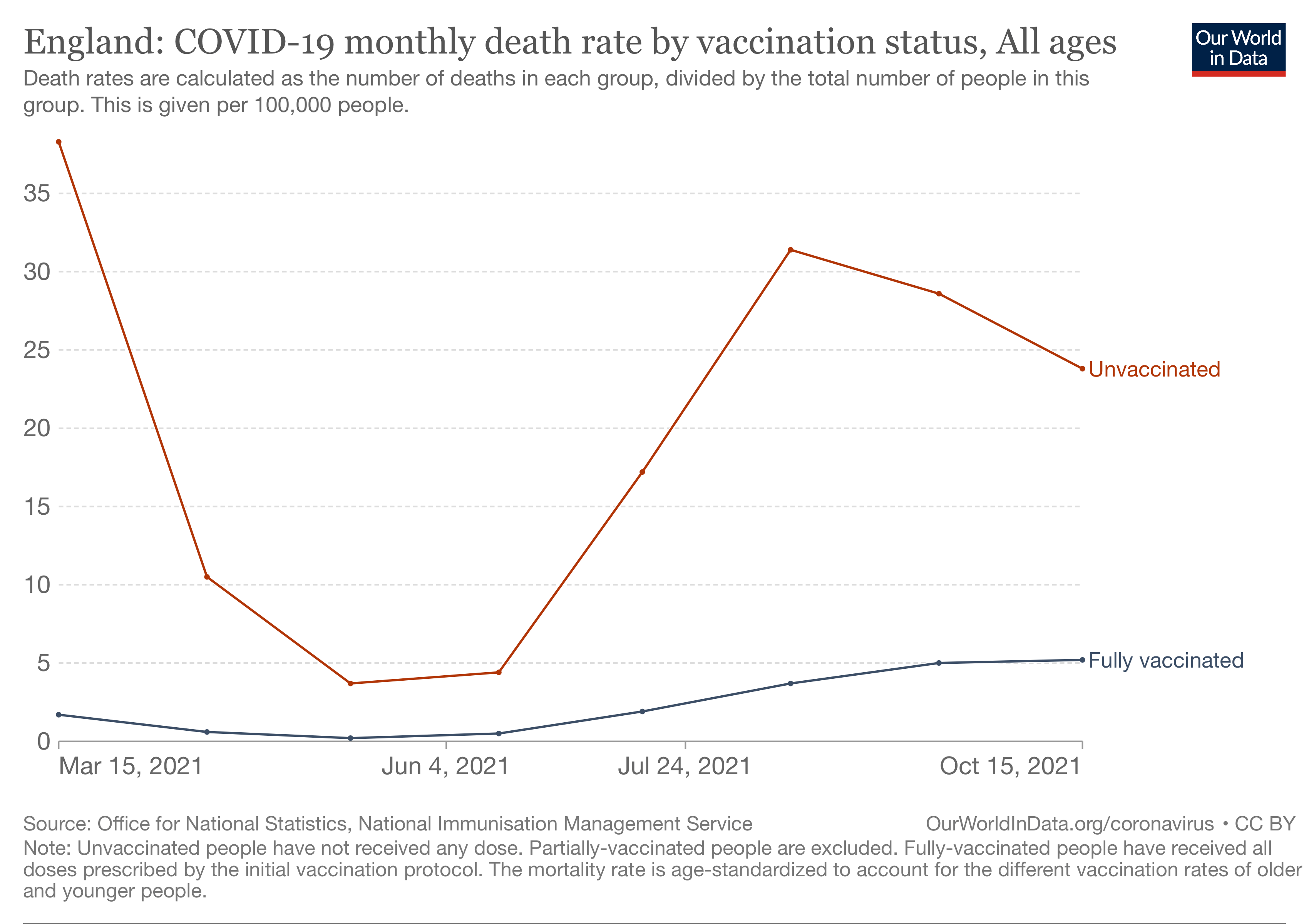
Figure 2. The COVID-19 weekly age-standardized mortality rate (per 100,000 people) in England based on vaccination status. Chart from Our World in Data. Retrieved on 24 August 2023.
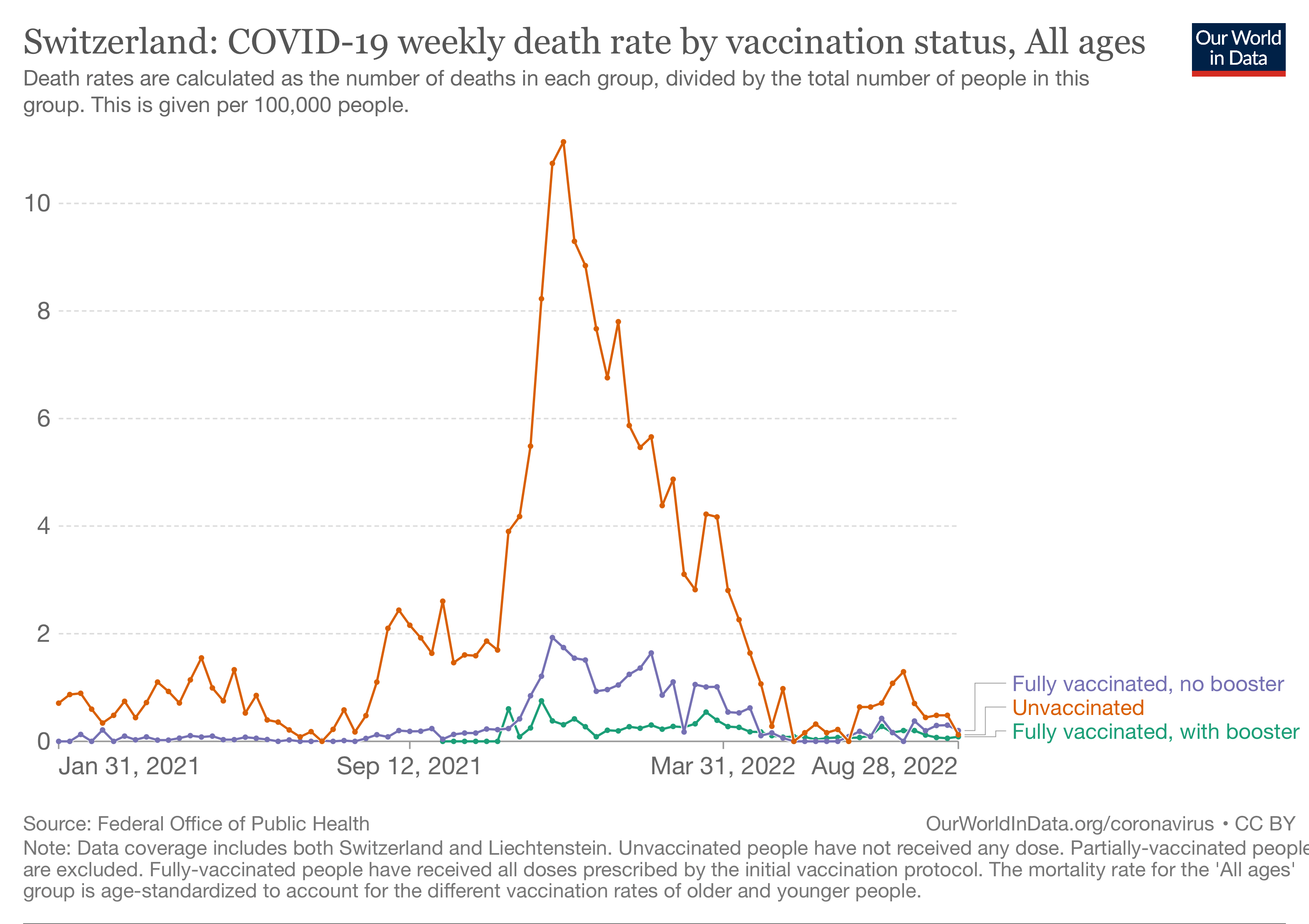
Figure 3. The COVID-19 age-standardized weekly mortality rate (per 100,000 people) in Switzerland based on vaccination status. Chart from Our World in Data. Retrieved on 24 August 2023.
Instagram posts’ focus on headlines strip important context from news articles
The January 2021 CNN article containing the headline “White people are getting vaccinated at higher rates than Black and Latino Americans” reported how this disparity at the beginning of the vaccination campaign was “[blamed] on the federal government and hospitals not prioritizing equitable access” by some public health advocates.
The October 2022 Washington Post article carrying the headline “Whites now more likely to die from covid than Blacks: Why the pandemic shifted” also doesn’t provide any support for the Instagram posts’ implication that COVID-19 vaccines were responsible for the rise in COVID-19 deaths in White people.
Actually reading the article would reveal that the data used in the Post’s analysis didn’t include COVID-19 mortality based on vaccination status. Therefore, it cannot be used to draw conclusions about differences in COVID-19 mortality between unvaccinated and vaccinated people. Nor did the article conclude that vaccinated people died from COVID-19 at a disproportionately higher rate than unvaccinated people.
While the CNN article reported a higher vaccination rate in White people when the COVID-19 vaccination campaign had just started—bearing in mind the article was published in January 2021—COVID-19 vaccine coverage in Black people eventually caught up with that in White people.
Supporting this is a study by researchers at the U.S. Centers for Disease Control and Prevention. They reported that by the end of November 2021, “disparities in vaccination coverage for some racial and ethnic groups narrowed, and coverage was similar for non-Hispanic Black (78.2%), Hispanic (81.3%), Native Hawaiian and other Pacific Islander (75.7%), and non-Hispanic White (78.7%) adults”[6].
Thus, this gap narrowing in vaccine coverage might go some way towards explaining the gap narrowing in COVID-19 mortality.
The Post article delved into several possible reasons why COVID-19 mortality in White people, which had initially been lower than that of other race groups (Hispanic, Black, Asian), gradually rose over time, occasionally even surpassing that of Black people.
We quote relevant segments in the article below to show what the article found to be some of the driving factors behind this shift in mortality
“After delta’s peak in September 2021, the racial differences in covid deaths started eroding. The Post analysis found that Black deaths declined, while White deaths never eased, increasing slowly but steadily, until the mortality gap flipped. From the end of October through the end of December, White people died at a higher rate than Black people did, The Post found.”
“The easy explanation is that it reflects the choices of Republicans not to be vaccinated, but the reasons go deeper. The Post interviewed historians and researchers who study the effects of White racial politics and social inequality on health, spoke with relatives and friends of those lost to covid, and compiled data from federal databases and academic studies.
What emerged is a story about how long-standing issues of race and class interacted with the physical and psychological toll of mass illness and death, unprecedented social upheaval, public policies — and public opinion.”
Studies document the disparity in COVID-19 mortality along racial, geographic, and party lines
Stark differences in the U.S. COVID-19 mortality along racial lines have been well-documented in the first year of the pandemic[7-11], with the White population generally experiencing a lower mortality rate compared to other racial groups, including Black people. Some reasons for this disparity include differences in access to healthcare, burden of chronic diseases like diabetes—which increase the risk of severe COVID-19—as well as socioeconomic status.
However, as the Post reported, this mortality gap narrowed later during the pandemic[12]. Ideologically- and politically-rooted differences in people’s acceptance of public health recommendations have been proposed as possible driving factors in the rise of COVID-19 mortality rate in White people. This was also a subject of discussion in the Post article, as the quotes above demonstrate.
Indeed, differences in COVID-19 mortality have been correlated with political partisanship. ABC News analyzed COVID-19 mortality rates in U.S. states and territories between 19 April 2021 and 1 March 2022. It found a marked difference in COVID-19 mortality rate and vaccine coverage depending on whether the state had voted for former president Donald Trump and those that voted for current president Joe Biden in the 2020 U.S. elections (Figure 4).
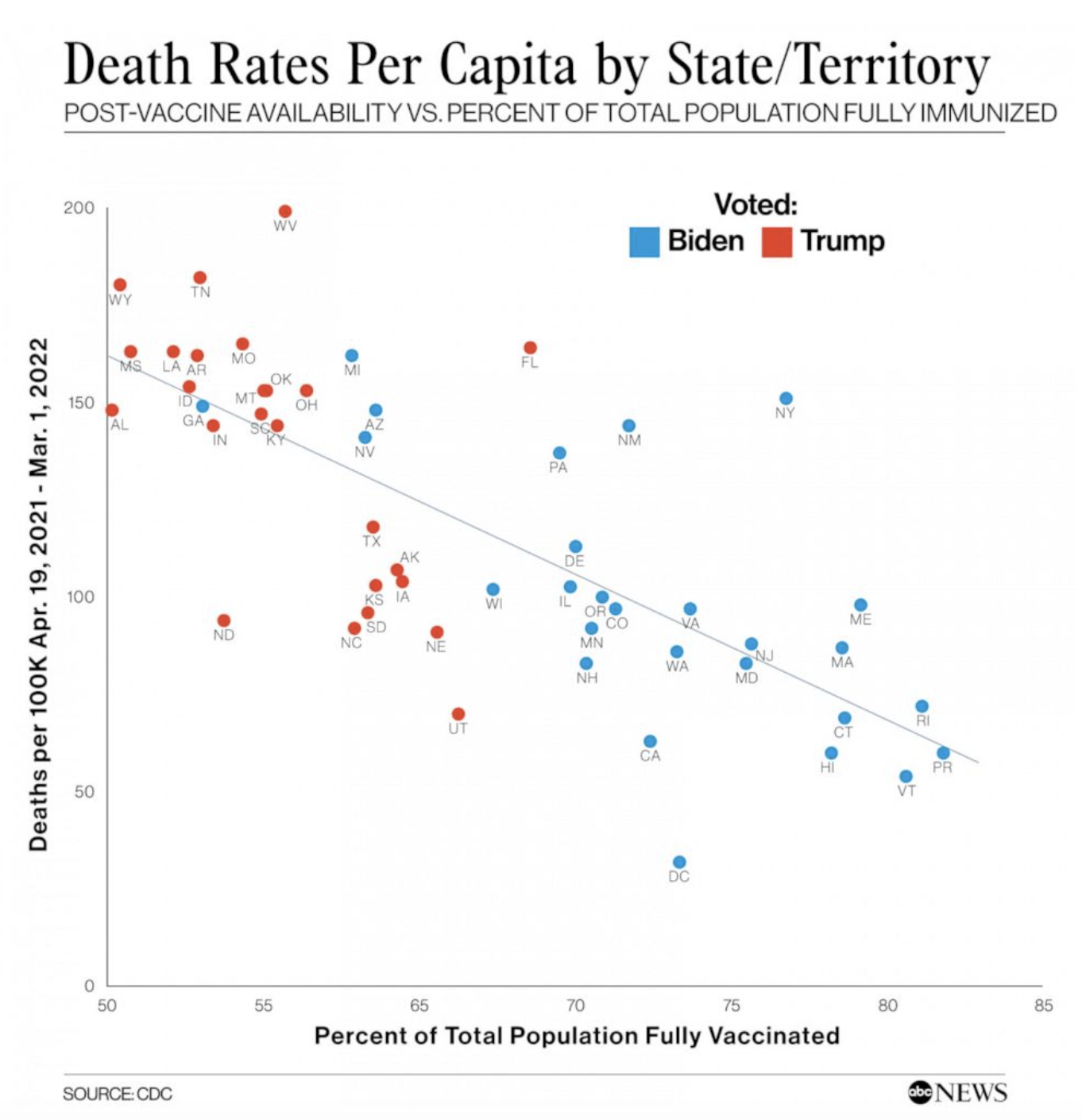
Figure 4. A graph showing a correlation between COVID-19 deaths, vaccine coverage, and which presidential candidate a state voted for. Source: ABC News.
As Figure 4 shows, states that voted for Trump tended to have higher COVID-19 mortality rates and lower vaccine coverage compared to states that voted for Biden.
But like the Post, ABC News didn’t analyze individual-level data on vaccination status and mortality, so this analysis alone cannot allow us to determine if the people who died of COVID-19 or got vaccinated disproportionately belonged to one camp or the other.
While it tells us that a difference in COVID-19 mortality and vaccine coverage along party lines does exist, it offers insufficient evidence to determine whether this difference is due to a causal relationship with political affiliation.
This is because Republican and Democratic-leaning states also differ from each other in terms of racial and ethnic composition, as well as rurality—the closure of rural hospitals due to underfunding has particularly limited rural healthcare access during the pandemic.
These factors are also associated with higher COVID-19 mortality[7-13]. In fact, they were already tied to health disparities even before the pandemic[14,15].
To better address the question of whether political affiliation can directly affect COVID-19 health outcomes, we can look to other analyses to complement the ABC News analysis.
For example, a report by the Kaiser Family Foundation, published in September 2021, gathered data about the public’s attitude towards COVID-19 vaccination and other recommendations. It found that 90% of Democrats polled received a COVID-19 vaccine dose. In contrast, just 58% of Republicans polled had received a dose.
The report also found that people’s opinion on mask-wearing, which helps reduce the spread of COVID-19, were also split along party lines. 83% of Democrats supported school mask mandates, while just 29% of Republicans supported such mandates. 60% of Republicans opposed any form of mask mandate.
There’s also a study by researchers at Yale that compared excess mortality rates between registered Republican and Democratic voters in Florida and Ohio[16]. They found that between March 2020 and December 2021, excess death rates were 15% higher for Republican voters compared with Democratic voters. After COVID-19 vaccines became available, the gap in excess death actually widened. However, this study is limited as it only included data from two states, raising questions about how generalizable its findings are.
Nevertheless, when taken together, these findings suggest that political affiliation does influence one’s risk of dying from COVID-19 and whether a person follows public health recommendations to reduce the spread of COVID-19.
Having said that, political affiliation isn’t the only determinant of COVID-19 mortality risk. As discussed above, racial and geographic factors also influence COVID-19 mortality risk. It’s important to keep in mind that these can interact with political affiliation, and that understanding shifts in mortality requires accounting for this complex interplay of race, geography, and politics—rather than a single factor.
Conclusion
In summary, the Instagram posts implying that a rise in COVID-19 deaths in White people was due to COVID-19 vaccination don’t stand up to scrutiny.
Research has shown that COVID-19 disproportionately affects people based on a combination of race, geography (urban vs. rural), as well as socioeconomic status. Intersecting with these factors are ideological and political positions, which influence people’s decisions to follow public health recommendations—like getting vaccinated—and in turn influence their risk of dying from COVID-19. Multiple scientific studies and population-level analyses have established that COVID-19 vaccination reduces the risk of severe disease and death.
REFERENCES
- 1 – Polack et al. (2020) Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. New England Journal of Medicine.
- 2 – Baden et al. (2021) Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. New England Journal of Medicine.
- 3 – Bernal et al. (2021) Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ.
- 4 – Taib et al. (2022) Characterisation of COVID-19 deaths by vaccination types and status in Malaysia between February and September 2021. The Lancet Regional Health – Western Pacific.
- 5 – Yan et al. Effectiveness of BNT162b2 and CoronaVac vaccinations against mortality and severe complications after SARS-CoV-2 Omicron BA.2 infection: a case–control study. Emerging Microbes and Infections.
- 6 – Kriss et al. (2022) COVID-19 Vaccination Coverage, by Race and Ethnicity — National Immunization Survey Adult COVID Module, United States, December 2020–November 2021. Morbidity and Mortality Weekly Report.
- 7 – Bassett et al. (2020) Variation in racial/ethnic disparities in COVID-19 mortality by age in the United States: A cross-sectional study. PLoS Medicine.
- 8 – Millett et al. (2020) Assessing differential impacts of COVID-19 on black communities. Annals of Epidemiology.
- 9 – Andrasfay and Goldman. (2021) Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. PNAS.
- 10 – Mude et al. (2021) Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: A systematic review and meta-analysis. Journal of Global Health.
- 11 – Kullar et al. (2020) Racial Disparity of Coronavirus Disease 2019 in African American Communities. Journal of Infectious Diseases.
- 12 – Lundberg et al. (2023) COVID-19 Mortality by Race and Ethnicity in US Metropolitan and Nonmetropolitan Areas, March 2020 to February 2022. JAMA Network Open.
- 13 – Monnat SM. (2022) Rural-Urban Variation in COVID-19 Experiences and Impacts among U.S. Working-Age Adults. Annals of the American Academy of Political and Social Science.
- 14 – Elo et al. (2019) Trends in Non-Hispanic White Mortality in the United States by Metropolitan-Nonmetropolitan Status and Region, 1990–2016. Population and Development Review.
- 15 – James et al. (2017) Racial/Ethnic Health Disparities Among Rural Adults — United States, 2012–2015. Morbidity and Mortality Weekly Report.
- 16 – Wallace et al. (2023) Excess Death Rates for Republican and Democratic Registered Voters in Florida and Ohio During the COVID-19 Pandemic. JAMA Internal Medicine.